Dr Karen Sennett Highlights Key Learning Points for Primary Care from the Updated NICE Guideline on Chronic Obstructive Pulmonary Disease (COPD)
| Read This Article to Learn More About: |
|---|
Find implementation actions for STPs, ICSs, and clinical pharmacists in general practice at the end of this article |
In the UK, around 1.2 million people have a diagnosis of chronic obstructive pulmonary disease (COPD) and many more may have the condition but be undiagnosed.1,2 COPD is a significant cause of emergency admissions and one of the most expensive inpatient conditions for the NHS.2 It is treatable but not curable and is usually progressive. About 30,000 people each year die of the condition, accounting for 5% of all UK deaths.2
NICE updated NICE Guideline (NG) 115 on Chronic obstructive pulmonary disease in over 16s: diagnosis and management in July 2019. New evidence has emerged and practice has changed regarding the use of inhaled triple therapy and oral corticosteroids so the updated guideline includes new recommendations on:1
- inhaled triple therapy for stable COPD
- systemic corticosteroids for managing exacerbations.
The guideline was also updated in 2018 to include revised advice on self-management, lung surgery, and education. Alongside the recommendations, primary care healthcare professionals may find it useful to refer to:3
- the five ‘fundamentals’ of COPD care
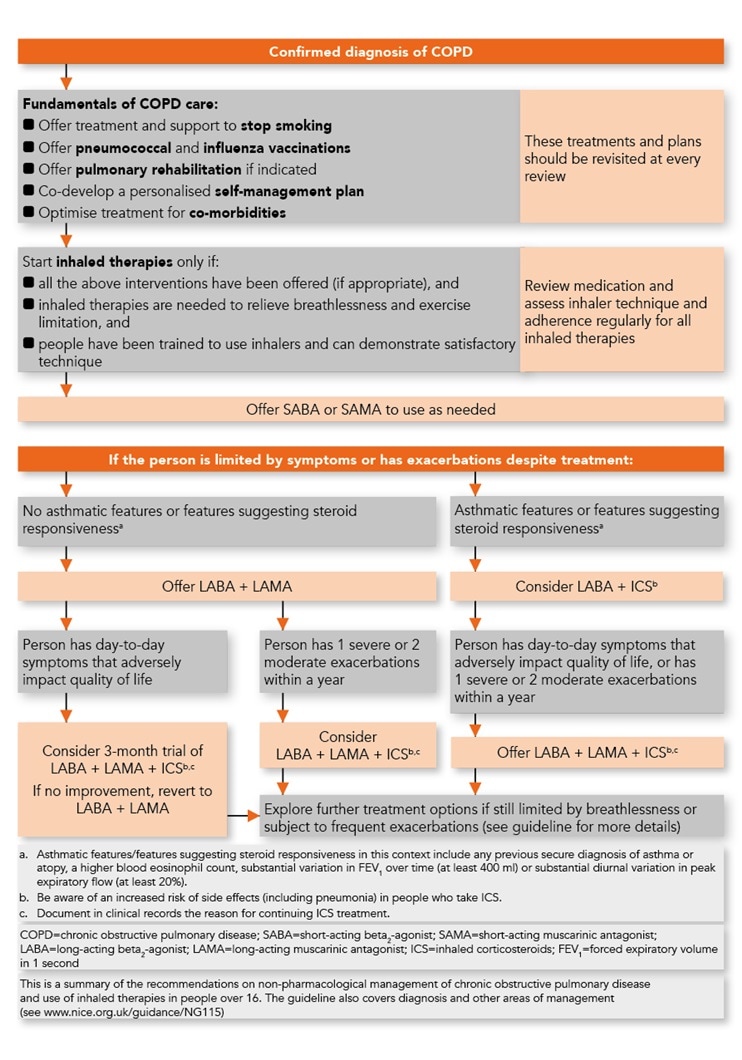
- a new NICE algorithm on non-pharmacological management and use of inhaled therapies in COPD (see Figure 1).
This article focuses on the recommendations from the July 2019 update that are relevant to healthcare professionals working in primary care. Readers may find it helpful to refer to the relevant NICE guideline alongside this article; recommendation numbers have been included [in brackets] to help you to locate the relevant place in the guideline.
Note: Not all of the treatments discussed in this article currently (October 2019) have UK marketing authorisation. Advice and safety alerts about certain treatments are also referenced in notes to NICE recommendations. The prescriber should follow relevant professional guidance, taking full responsibility for all clinical decisions. Informed consent should be obtained and documented. See the General Medical Council’s guidance on Good practice in prescribing and managing medicines and devices4 for further information.
© NICE 2019 Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Available from www.nice.org.uk/guidance/ng115 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
1. Follow the Five ‘Fundamentals’ of COPD Care
Think about the following with the patient at every review:1,3
- offer treatment and support to stop smoking (this is the highest value intervention—cover at every clinical contact)
- offer pneumococcal and influenza vaccination
- offer pulmonary rehabilitation for people who have functional impairment (Medical Research Council [MRC] dyspnoea scale ≥3)
- co-develop a personalised self-management plan with the patient
- optimise treatment for co-morbidities—ensure that these are identified and then treated.
2. Know How to Diagnose COPD
Suspect a diagnosis of COPD in anyone with a history of exertional breathlessness, chronic cough or regular sputum production, frequent winter bronchitis, or wheeze, with risk factors including a history of tobacco smoking or working in an occupation with exposure to chemicals or dust.1,2
It is useful to perform spirometry [see NG115; 1.1.4 and 1.1.12]:1
- at diagnosis
- to monitor disease progression
- to reconsider the diagnosis, e.g. if a person shows an exceptionally good response to treatment
- for a person who has a chest X-ray or computed tomography (CT) scan performed for another reason that shows signs of emphysema or chronic airways disease (see heading 4, below).
The diagnosis of COPD is based on the presence of airflow obstruction, usually defined as a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of <0.7, measured using spirometry.
Distinguishing between COPD and asthma can be challenging and is particularly important when it comes to choosing appropriate inhaled therapies (see text under heading 6, ‘Prescribe and escalate inhaled therapies as appropriate’, below). The NICE recommendations on how to differentiate between COPD and asthma are largely unchanged since 2004.
3. Give the Patient Written Information
At diagnosis and at review appointments, in primary or secondary care:1
- offer people with COPD and their family members or carers:
- accessible written information (e.g. British Lung Foundation COPD materials)5 tailored to their needs. NICE provides a detailed list of the minimum information required (see Box 1)
- an opportunity for discussion with a health professional who has experience in caring for people with COPD
- co-develop an individualised self-management plan, inclusive of the information in Box 1. If the person with COPD is at risk of exacerbations, co-develop an individualised exacerbation management action plan too (see heading 7).
| Box 1: Written Information for People with COPD1 |
|---|
At minimum, the information should cover:
COPD=chronic obstructive pulmonary disease © NICE 2019. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Available from www.nice.org.uk/ng115 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this publication. |
4. Know How to Manage Incidental Findings on X-ray or CT Scan
For patients who have incidental findings of emphysema or chronic airways disease on a chest X-ray or CT scan, primary care review of their respiratory symptoms and also spirometry should be considered [see NG115; 1.1.12].1
If spirometry is normal, if they have no symptoms or signs of respiratory disease, and they are a current smoker [see NG115; 1.1.13]:1
- offer smoking cessation advice and treatment, and referral to specialist stop smoking services (see NG92 on Stop smoking interventions and services6)
- warn them that they are at higher risk of lung disease
- advise them to return if they develop respiratory symptoms
- be aware that the presence of emphysema on a CT scan is an independent risk factor for lung cancer.
If the spirometry is normal, if they have no symptoms or signs of respiratory disease, and they are not a current smoker [see NG115; 1.1.14]:1
- ask them if they have a personal or family history of lung or liver disease and consider alternative diagnoses, such as alpha‑1 antitrypsin deficiency
- reassure them that their emphysema or chronic airways disease is unlikely to get worse
- advise them to return if they develop respiratory symptoms
- be aware that the presence of emphysema on a CT scan is an independent risk factor for lung cancer.
5. Know What Investigations to Offer Patients
All patients newly diagnosed with COPD should have a [see NG115; 1.1.15]:1
- chest radiograph to exclude other pathologies
- full blood count in case of anaemia or polycythaemia
- calculation of body mass index.
Other investigations may be needed in some patients, for example:
- testing for serum alpha-1 antitrypsin deficiency if there is early onset, minimal smoking history, or a family history of that condition
- serial home peak flow readings to exclude asthma if diagnostic doubt remains.
See Table 2, ‘Additional investigations’ in NICE NG115 for other possible investigations.1
6. Prescribe and Escalate Inhaled Therapies as Appropriate
Start inhaled therapies (short-acting beta2 -agonists [SABA] or short-acting muscarinic antagonists [SAMA]) only if:1,3
- the ‘five fundamentals’ (see Figure 1) have been offered as appropriate
- inhaled therapies are needed to relieve breathlessness and exercise limitation
- the patient has been trained to use inhalers.
Escalating inhaled therapies. If the person remains breathless or has exacerbations despite using a SABA or SAMA inhaler, and the five ‘fundamentals’ have been offered (where appropriate), the next step depends on whether or not the person also has asthmatic features or features suggesting steroid responsiveness:1,3
- if there are no asthmatic features offer combined long-acting beta2 -agonists (LABA) + long-acting muscarinic antagonists (LAMA)
- if there are asthmatic features consider LABA + inhaled corticosteroids (ICS).
NICE defines ‘asthmatic features/features suggesting steroid responsiveness’ as ‘any previous, secure diagnosis of asthma or of atopy, a higher blood eosinophil count, substantial variation in FEV1 over time (at least 400 ml) or substantial diurnal variation in peak expiratory flow (at least 20%).’1
Details about further escalation of treatment (triple therapy) are provided in NG115 and summarised in Figure 1.1,3 Triple therapy should only be started after a clinical review and in accordance with recommendations 1.2.14 onwards in the updated guideline.
NB Patients with COPD alone (no asthmatic features or features suggesting steroid responsiveness) who are taking LAMA + LABA and whose day-to-day symptoms are adversely impacting their quality of life can be considered for a 3-month trial of triple therapy (LAMA + LABA + ICS). If their symptoms improve, the triple therapy treatment can be continued (document the reason at least once yearly); if there is no improvement after 3 months, revert to dual therapy.1,3 Refer to the guideline for more detail [see NG115; 1.2.14 onwards].1
7. Plan For and Treat Exacerbations
The guideline [see NG115; 1.2.125] recommends developing an individualised exacerbation plan with each patient with COPD who is at risk of exacerbations. It also recommends [see NG115; 1.2.126] offering the person a short course of oral corticosteroids and a short course of oral antibiotics to keep at home as part of their exacerbation action plan if:1
- they have had an exacerbation within the last year, and remain at risk of exacerbations
- they understand and are confident about when and how to take these medicines, and the associated benefits and harms
- they know to tell their healthcare professional when they have used the medicines, and to ask for replacements.
Use of corticosteroids and antibiotics kept at home should be discussed with the patient at every review and reasons for three or more courses taken in 1 year investigated [see NG115; 1.2.128].1
The guideline recommends 5 days’ treatment with oral prednisolone 30 mg daily when needed for acute exacerbations [see NG115; 1.3.16]; evidence shows no benefit from courses longer than 7 days and 5-day courses are routinely used in clinical practice.1 Antibiotics can also be offered as appropriate, see below.
Prescribing Antibiotics
For acute exacerbations of COPD, antibiotics can be offered for 5 days if needed;7 a 5-day course is now recommended because there was no evidence of benefit from longer courses and there are significantly fewer adverse events with short-course antibiotics than with long courses.7 Bear in mind that many exacerbations (including some severe exacerbations) are not caused by bacterial infections and will therefore not respond to antibiotics.7 NICE recommends:
- consider an antibiotic [see NG115; 1.2] for people with an acute exacerbation of COPD, but only after taking into account:1
- the severity of symptoms, particularly sputum colour changes and increases in volume or thickness beyond the person’s normal day-to-day variation
- whether they may need to go into hospital for treatment
- previous exacerbation and hospital admission history, and the risk of developing complications
- previous sputum culture and susceptibility results
- the risk of antimicrobial resistance with repeated courses of antibiotics
- give oral antibiotics first line if the person can take oral medicines, and the severity of their exacerbation does not require intravenous antibiotics [see NG114; 1.2.2]7
- refer people with an acute exacerbation of COPD to hospital if they have any symptoms or signs suggesting a more serious illness or condition [see NG114; 1.1.7].7
See NG114 on Chronic obstructive pulmonary disease (acute exacerbation): antimicrobial prescribing for further detailed information.
Bronchiectasis
Mucus build-up in patients with bronchiectasis can increase susceptibility to infection,8 and antibiotic courses longer than 5 days (7–14 days) are recommended by NICE for people with acute exacerbations of bronchiectasis (see NG117 on Bronchiectasis [non-cystic fibrosis], acute exacerbation: antimicrobial prescribing).9 There are no specific recommendations in NG115 or NG117 for prescribing antibiotics for exacerbations in patients with both COPD and bronchiectasis.
Prophylactic Antibiotics in People with Frequent Exacerbations
Regular azithromycin therapy (usually 250 mg three times a week) can be beneficial in some patients who do not smoke (as it is ineffective in continued smokers) and who have a substantial exacerbation burden despite having optimised non-pharmacological management and inhaled therapies, relevant vaccinations, and pulmonary rehabilitation (if appropriate). A substantial exacerbation burden is defined as people who continue to have one or more of the following, particularly if they have significant daily sputum production [see NG115; 1.2.46]:1
- frequent (typically four or more per year) exacerbations with sputum production
- prolonged exacerbations with sputum production
- exacerbations resulting in hospitalisation.
The following criteria should have been met before starting prophylactic antibiotics:1,3
- consider whether respiratory specialist input is needed [see NG115; 1.2.45]
- ensure the person has had [see NG115; 1.2.47]:
- sputum culture (including for tuberculosis), to identify other possible causes of persistent or recurrent infections
- training in airway clearance techniques to optimise sputum clearance
- CT scan of the thorax to rule out bronchiectasis or other lung pathology.
Before starting azithromycin ensure the person has had [see NG115; 1.2.48]:1
- an electrocardiogram (ECG) to rule out prolonged QT interval and
- baseline liver function tests.
The person should also receive a warning about the small risk of hearing loss and tinnitus from azithromycin and be advised to contact their health professional if this occurs.1
Ensure that the patient receives follow-up review at 3 months then at least every 6 months and only continue if the benefits outweigh the risks; the longest follow up in trials was 12 months, so there is currently no evidence on the long-term effects of prophylactic antibiotics on people with COPD.1
Patients who are taking prophylactic azithromycin may also keep antibiotics at home as part of their exacerbation action plan (see text above and NG115, 1.2.126).1 This should be a different class of antibiotic from azithromycin to ensure that it is effective, as the person may develop resistance to azithromycin. The prophylactic azithromycin may be continued during the acute exacerbation.1
8. Know When to Consider Oxygen Therapy
Long-term Oxygen Therapy
Continuous long-term home oxygen therapy (LTOT), for a minimum 15 hours per day, can improve survival in people with COPD who have more severe hypoxaemia.1 The guideline states [see NG115; 1.2.58] that LTOT can be considered in people who do not smoke and who have:1
- a partial pressure of oxygen in arterial blood (PaO2) of less than 7.3 kPa when stable or
- a PaO2 above 7.3 kPa and below 8 kPa in the presence of one or more of:
- secondary polycythaemia
- peripheral oedema
- pulmonary hypertension.
Patients being considered for LTOT should have a firm diagnosis of COPD and be receiving optimum medical management for their condition, which should be stable. Their blood gases should be measured on two occasions at least 3 weeks apart.1
Risk Assessment for Long-term Oxygen Therapy
Potential risks to the patient and others can arise from the use of long-term oxygen therapy, e.g. burns and fires as a result of smoking while using oxygen, and falls from tripping over equipment. It is therefore important to conduct a structured risk assessment before offering LTOT.1 People who meet the criteria for LTOT but who smoke (or who live with people who smoke) should be offered smoking cessation advice and treatment, and referral to specialist stop smoking services.1
For those patients who continue to smoke, NICE’s recommendation [see NG115; 1.2.61] is:1
- do not offer long-term oxygen therapy to people who continue to smoke despite being offered smoking cessation advice and treatment, and referral to specialist stop smoking services.
For people who do not themselves smoke but who live with someone who smokes, the risk may (subject to risk assessment) be lower because the person who smokes may be able to keep away from the oxygen.
Ambulatory Oxygen Therapy
Ambulatory oxygen therapy needs respiratory specialist assessment before it is started.1 Ambulatory oxygen can be considered for people with COPD who, on assessment by a specialist, have exercise desaturation and are shown to have an improvement in exercise capacity with oxygen; they should also have the motivation to use oxygen.1
Evidence shows that neither ambulatory oxygen nor short-burst oxygen provides a clinically meaningful improvement in breathlessness for people with mild or no hypoxaemia.1 Short-burst oxygen to manage breathlessness for people with COPD, who have mild or no hypoxaemia at rest, should not be offered [see NG115; 1.2.73].1
9. Know When to Refer for Possible Lung Volume Reduction
The evidence for lung volume reduction (LVR) surgery or endobronchial valve replacement now shows benefit in certain individuals with COPD, with improvements in lung function, exercise capacity, quality of life and long-term mortality.1
At the end of pulmonary rehabilitation and at other reviews, offer a respiratory review for surgery if all the following apply [see NG115; 1.2.88]:1
- FEV1 <50%
- quality of life is limited by breathlessness despite optimal treatment [see NG115; 1.2.11 to 1.2.17]
- the patient does not smoke
- the patient is able to walk a distance of at least 140 metres in 6 minutes.
A specialist lung volume reduction multidisciplinary team will assess the patient’s suitability for surgery.1
10. Make an Action Plan for COPD in Your Own Practice
Develop a plan for managing patients with COPD in your practice, supported and informed by the recommendations in the NICE guideline. For example:
- ensure that all patients with COPD get access to the five ‘fundamentals’ from all GPs, practice nurses, and pharmacists in your practice
- make sure that staff who perform or interpret spirometry are adequately trained and that their knowledge is up to date
- find a way to ensure that all your patients with COPD are on the correct medication
- make sure that all your clinical staff are trained in offering (or signposting to) smoking cessation treatments, e.g. the National Centre for Smoking Cessation and Training (NCSCT) very brief advice (VBA) online learning (which takes 15 minutes)10
- develop a system to review patients who are using rescue packs of steroids and antibiotics more than three times a year; should they be on current, not repeat, medication lists so there is an opportunity to review?
Dr Karen Sennett
GP, Killick Street Health Centre, London; Islington CCG COPD lead GP; NICE COPD Committee member
The guideline referred to in this article was produced by the Guideline Updates Team for the National Institute for Health and Care Excellence (NICE). The views expressed in this article are those of the authors and not necessarily those of NICE.
National Institute for Health and Care Excellence (2019) Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Available from: www.nice.org.uk/guidance/ng115
| Implementation Actions for STPs and ICSs |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved with implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
STP=sustainability and transformation partnership; ICS=integrated care system; MRC=Medical Research Council dyspnoea scale; QOF=quality and outcomes framework; COPD=chronic obstructive pulmonary disease |
| Implementation Actions for Clinical Pharmacists in General Practice |
|---|
Written by Gupinder Syan, Training and Clinical Outcomes Manager, Soar Beyond Ltd The following implementation actions are designed to support clinical pharmacists in general practice with implementing the guidance at a practice level.
COPD=chronic obstructive pulmonary disease; LABA=long-acting beta2 -agonist; LAMA=long-acting muscarinic antagonist |

