Dr Kevin Gruffydd-Jones Identifies Six Key Learning Points for Primary Care from the British Thoracic Society Guideline on Bronchiectasis
| Read This Article to Learn More About: |
|---|
Find Key points, COVID-19 considerations, and implementation actions for STPs and ICSs at the end of this article |
Bronchiectasis is a chronic condition in which irreversible damage to and dilation of the bronchi lead to symptoms of persistent or recurrent bronchial sepsis.1 A GP practice of 10,000 patients will have around 50 adult patients with bronchiectasis.2
The British Thoracic Society guideline for bronchiectasis in adults was published in 2019.3 The implications of this guidance for primary care were set out in an article targeted at a specialist global primary care audience.1 This article outlines the key points for primary care from the guideline and from the summary article for primary care.
1. Learn to Recognise and Diagnose Bronchiectasis
A diagnosis of bronchiectasis should be suspected in patients with a recurrent or persistent cough that has lasted for more than 8 weeks and features the production of purulent or mucopurulent sputum.1,3 There should be a lower index of suspicion for bronchiectasis if there are co-existing factors, as outlined in Box 1.2 In particular, a study of UK general practices showed the presence of bronchiectasis in 29% of patients aged 40–80 years who presented to their GP with an acute exacerbation of chronic obstructive pulmonary disease (COPD).4
| Box 1: Co-existing Conditions Raising the Probability of Bronchiectasis in Patients Presenting with Chronic, Productive Cough2 |
|---|
COPD=chronic obstructive pulmonary disease; FEV1 =forced expiratory volume in 1 second; P. aeruginosa =Pseudomonas aeruginosa |
Although it was an element that was not covered by the British Thoracic Society (BTS) guideline, healthcare professionals should consider whether the patient has COVID-19 or a history of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (see COVID-19 considerations box at the end of this article). For more information on the long-term effects of COVID-19, refer to guidance issued by NICE and the Primary Care Respiratory Society.5,6
To exclude other causes of chronic cough, such as COPD, asthma, lung cancer, or gastro-oesophageal reflux, a full history should be taken and an examination conducted.1 In patients with bronchiectasis, examination of the chest may or may not reveal the presence of characteristic persistent inspiratory basal crackles.1 The upper airway should be examined for the presence of chronic rhinosinusitis.3
Investigations should include a chest X-ray (which may be normal), diagnostic spirometry (which may be normal, restrictive, or obstructive), and sputum culture to identify persistent pathogens, such as Pseudomonas aeruginosa (the presence of which indicates a worse prognosis).1,3
Definitive diagnosis of bronchiectasis is carried out by thin-section computed tomography (CT) scanning of the chest.1,3 This may be arranged by direct access or via specialist referral.
Figure 1 shows a proposed algorithm for the diagnosis of bronchiectasis after presentation in primary care.1
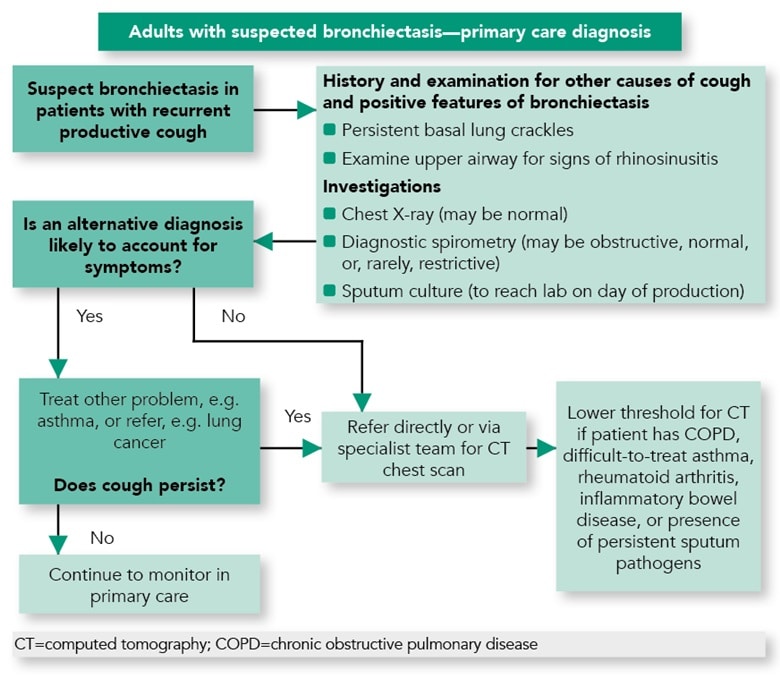
Gruffydd-Jones K, Keely D, Knowles V et al. Primary care implications of the British Thoracic Society Guidelines for bronchiectasis in adults 2019. NPJ Prim Care Respir Med 2019; 29: 24.Reproduced with permission. Available under the CC-BY 4.0 licence.
2. Know When to Refer to a Specialist
Once a firm diagnosis is made, it is recommended that the initial assessment should be conducted by a specialist respiratory team in order to elucidate any underlying causes, evaluate any co-morbid conditions, and formulate a joint management plan. This assessment should take into consideration details of routine treatment, investigations, place of routine review, and actions to take in case of flare up, including relevant contact details.1
A proposed algorithm for the review and management of patients with bronchiectasis in primary care is provided in Figure 2.1
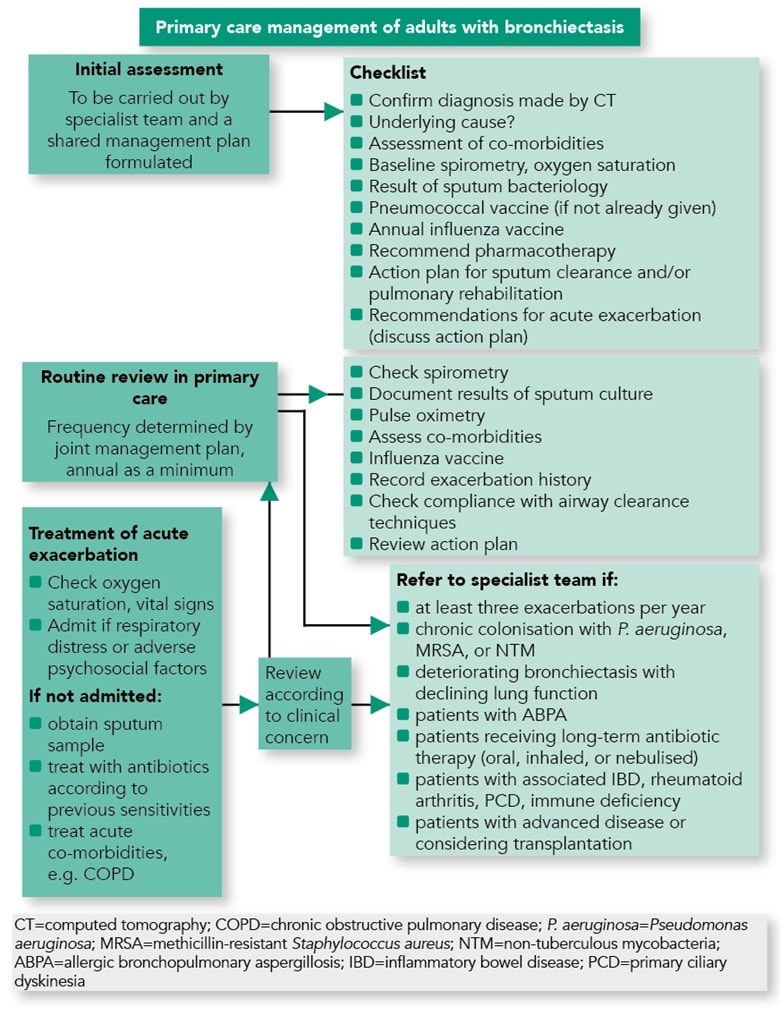
Gruffydd-Jones K, Keely D, Knowles V et al. Primary care implications of the British Thoracic Society Guidelines for bronchiectasis in adults 2019. NPJ Prim Care Respir Med 2019; 29: 24.Reproduced with permission. Available under the CC-BY 4.0 licence.
3. Understand the Aims of Management
The overall aims of the management of bronchiectasis are to prevent further lung damage, maximise lung function and quality of life, and prevent and treat exacerbations.1 The cornerstones of management are summarised in Box 2.
| Box 2: Cornerstones of Bronchiectasis Management |
|---|
[A] Treatment with inhaled corticosteroids should not be routinely offered to patients with bronchiectasis without other indications (such as COPD or asthma). There is no evidence to support the use of short-acting beta-2 agonists, although it is recommended to offer a trial, usually lasting 6 months, of long-acting inhaled bronchodilators in patients with significant breathlessness. If the patient benefits, the bronchodilator should be continued.3 COPD=chronic obstructive pulmonary disease |
Physiotherapy
All patients with bronchiectasis should be assessed by a respiratory physiotherapist.3 Chest physiotherapy can mobilise secretions and aid effective expectoration, providing an improvement in cough scores.1
Figure 2 shows the key physiotherapeutic interventions for bronchiectasis.1 In addition, some excellent downloadable videos on chest clearance techniques are available at bit.ly/3qOQ np7.
Long-term Antibiotic Therapy
Long-term antibiotic therapy—that is, antibiotic therapy lasting for 3 months or more—should be considered for patients who experience three or more exacerbations per year, and this treatment should be initiated and monitored by specialists in secondary care.1 The BTS guideline recommends a starting dose of azithromycin 250 mg, to be taken orally three times a week for 1 year, to reduce the incidence of exacerbations in these patients with bronchiectasis.1,3 A recent two-step meta-analysis of long-term macrolide therapy (published pre-peer review) found that the frequency of exacerbations was reduced by 51% in patients with two or more exacerbations per year, irrespective of whether they were colonised with P. aeruginosa.8 Patients whose symptoms do not respond to long-term antibiotic therapy with azithromycin, or in whom macrolides are contraindicated, may be offered long-term inhaled antibiotic therapy (such as colistin or gentamicin) or long-term intravenous antibiotics.1,3
4. Know When to Refer Patients to Secondary Care
Patients should be referred to secondary care for:
- access to diagnostic CT scanning (if direct access is not available)
- initial assessment after diagnosis (see Box 1).
Patients should also be referred to secondary care if their bronchiectasis is established and they have any of the following:1
- three or more exacerbations per year
- chronic colonisation with P. aeruginosa, methicillin-resistant Staphylococcus aureus, or non-tuberculous mycobacteria
- allergic bronchopulmonary aspergillosis
- long-term antibiotic therapy (oral, inhaled, or nebulised)
- associated inflammatory bowel disease, rheumatoid arthritis, primary ciliary dyskinesia, or immune deficiency
- advanced disease, or are considering transplantation
- deterioration of lung function.
5. Conduct a Routine Review in Primary Care
Patients will have been assessed by the specialist team as suitable for review in primary care, and the frequency of review will be stated in the management plan (but will be annual as a minimum).
The key elements of this routine review are to:1
- check spirometry (for evidence of disease deterioration and co-morbid airway disease)
- ensure that a recent sputum culture has been conducted
- perform pulse oximetry
- assess co-morbidities, such as asthma and COPD
- check that pneumococcal and annual influenza vaccinations have been given
- record exacerbation history
- check compliance with airway clearance techniques (if in doubt, re-refer to physiotherapy)
- review the patient’s action plan.
Although not covered by the BTS guideline, healthcare professionals should also consider whether patients have been vaccinated against COVID-19.
6. Manage Acute Flare Ups
Initial assessment should determine if a patient needs urgent hospital admission. Hospital admission should be considered if the patient is experiencing respiratory distress, exhibiting features of sepsis, or has significant co-morbidities.1
Ideally, patients who are managed in primary care should have a sputum sample taken prior to antibiotic treatment.1 If suitable, patients should be provided with antibiotics to keep at home.
Choice of antibiotic will be determined by culture and local sensitivities; if not known, empirical treatment should be started with amoxicillin 500 mg three times daily (doxycycline 100 mg twice daily if allergic to penicillin) or ciprofloxacin 500 mg twice daily if P. aeruginosa infection has been identified (750 mg twice daily for severe infection) while awaiting the results of sputum culture.1 Most patients with moderate and severe bronchiectasis should undergo 14 days of antibiotic therapy, although in patients with mild bronchiectasis a 7–10-day course may suffice.1
Advice to aid expectoration should be reinforced, and the treatment plan should be reviewed, especially the need for re-referral for physiotherapy or to secondary care.
Kevin Gruffydd-Jones
GP, Box, Wiltshire
| COVID-19 Considerations |
|---|
|
| Key Points |
|---|
CT=computed tomography; COPD=chronic obstructive pulmonary disease; P. aeruginosa=Pseudomonas aeruginosa |
| Implementation Actions for STPs and ICSs |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved in implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
STP=sustainability and transformation partnership; ICS=integrated care system; CT=computed tomography |

