Garry McDonald Describes the Key Elements of an Asthma Annual Review and Explains how Practice Pharmacists Can Support Asthma Management in Primary Care
| Read This Article to Learn More About: |
|---|
|
Asthma still kills each year, despite being a treatable and manageable disease. Every 10 seconds, someone in the UK experiences a potentially life-threatening asthma attack. In 2016, asthma was responsible for 1410 fatalities, and (tragically) around two-thirds of these deaths were preventable.1
In 2014, the National Review of Asthma Deaths (NRAD) published a report, Why asthma still kills.2 The 19 key recommendations outlined in the report should have been a wake-up call for healthcare professionals. Worryingly, it seems that as professionals, we are still fast asleep. Simply implementing the NRAD recommendations has been shown to reduce A&E admissions and deaths, and improve overall care and quality of life for patients.3
Practice-based pharmacists can play a crucial role in implementing many of the NRAD recommendations. This article will discuss where practice pharmacists fit into the multidisciplinary team, and how they can deliver care to people with asthma.
The Role of the Practice Pharmacist
It is important to remember that the role of the practice pharmacist is not as a GP substitute. Working within clinical competencies, a practice pharmacist will never diagnose; however, within their clinical competencies they can work right up to the wire once a diagnosis has been made, even challenging the diagnosis if it does not fit the disease picture.
So, where does a practice pharmacist begin when tackling asthma? Before even consulting with a patient, it’s invaluable to understand the practice landscape. As with any quality improvement, it’s vital to know where you are starting from before you know where you want to get to. Therefore, a few key reports should be created as a benchmark before undertaking any clinical work. Remember that asthma kills, so it should be a priority when conducting any respiratory reviews in practice.
Create Asthma Reports
SABA Usage
Simply identifying the number of short-acting beta2 agonists (SABAs) issued to all patients on the practice asthma register over a 12-month period will give a great snapshot of the current level of asthma control in the practice. Don’t be surprised if it looks very similar to the results from the NRAD report, with many patients issued more than 12 SABAs a year—one patient had over 100!2
Irrespective of which guideline (BTS/SIGN5 or NICE6) or strategy (GINA7) is being followed locally, a patient with well-controlled asthma should expect to have no more than three breathless moments a week (see the British Lung Foundation’s description of breathlessness8).2 Typically, each breathless moment requires relief with two doses from a SABA—a single pMDI (pressurised Metered Dose Inhaler) canister of salbutamol contains 200 doses—therefore just one SABA inhaler should be enough to last a year. Patients using more than one SABA inhaler a year have poorly controlled asthma, and patients using more than 12 a year are at significant risk of death.2 The International Primary Care Respiratory Group (IPCRG)9 and its UK affiliate the Primary Care Respiratory Society (PCRS)10 have developed a simple and effective tool as part of the Asthma Right Care initiative to illustrate SABA usage and over-dependence (see Figure 1).11
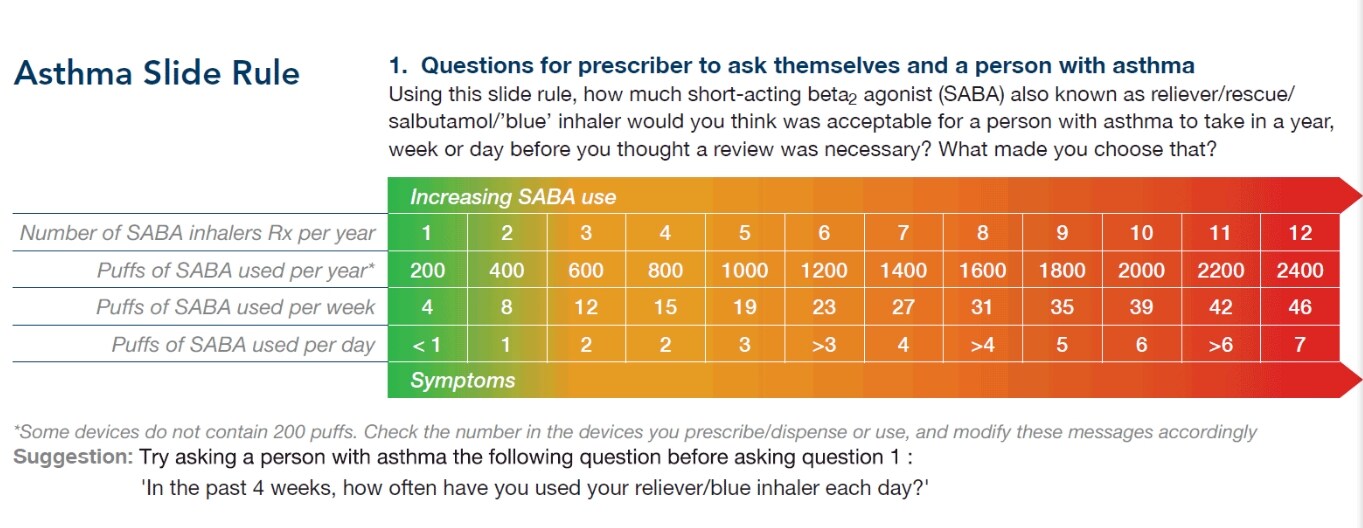
Primary Care Respiratory Society. Asthma Right Care (ARC). www.pcrs-uk.org/asthma-right-care (accessed 7 March 2019).
Reproduced and adapted under the terms of the CC BY-NC-SA 4.0 license
From this SABA usage report, a stratified work plan can be drawn up to target patients at the highest risk of death, such as those 39% of patients who died from asthma who had been issued with more than 12 SABAs in the preceding 12 months.2
SABA to ICS Ratio
Another fundamental report is to analyse the ratio of SABAs to inhaled corticosteroids (ICS) issued by the practice. An indicator of good practice would be around 1:6 (SABA:ICS); essentially one SABA issued every 6 months and one ICS issued every month (NB In theory, one SABA inhaler is enough to last for a year, however, in practice patients will usually need more [e.g. an extra one to keep at school/work or to replace one they have lost]. The 1:6 ratio is simply a target for good practice, not perfect practice). Current practice in the UK is two SABA inhalers issued for every ICS.12 In England, community pharmacists are incentivised to refer patients who have had more than six SABA inhalers and no ICS dispensed within a 6-month period.13 Community pharmacists are a useful ally in the management of asthma.
Integrating a few other markers in patient records can further target high-risk patients. Age, for example, is a risk factor in asthma. Recent Asthma UK data shows that 88% of ‘millennials’ (those born between 1980 and the early 2000s) with asthma have uncontrolled asthma, and are the most likely of all adults to present at A&E.14 The same report cites a ‘lack of a reminder’ as a reason why 60% of all patients do not attend an annual asthma review.14
Armed with a list of patients with asthma who are deemed to be at high risk of death, the next step is to convince these patients to attend the practice for an annual review, which is easier said than done. However, the relatively new role of the practice pharmacist can often stimulate patients to attend out of curiosity, and pharmacists tend to get a little more time per consultation than GPs. It is also worth trying to promote the consultation to the patient as an ‘MOT’ for their asthma. Invitations can be made by phone, email (where available), or text message. If the patient has not attended for a number of years, it may be beneficial to book longer or double appointment slots if possible.
Check Patient Records
Interrogation of patient notes and diagnosis is vital; a recent study showed that around one-third of coded asthma diagnoses were incorrect.15 With the variable nature of asthma, some patients can be asymptomatic for a considerable time. The original diagnosis may be questioned at a future date if it has not been detailed precisely and coded correctly in the notes. A list of asthma codes (and all other clinical codes) can be found on the University of Manchester’s ClinicalCodes website.16
As yet, there is not one simple diagnostic test for asthma. Given that there are a number of guidelines and strategies on the diagnosis and management of asthma,5–7 a structured, pragmatic consultation needs to be employed by all in the practice to prevent variation within the practice.17 The PCRS Consensus document is invaluable here as it provides clarity on aspects of diagnosis, management, and monitoring of asthma that are uncertain due to differences between current national guidelines.18
The scope of this article is not to explain the clinical diagnosis or pathophysiology of asthma, expert clinicians have covered this in previous Guidelines in Practice articles.19–21
Perform an Asthma Review
A practice pharmacist is well placed to carry out a structured, pragmatic annual asthma review. Bearing in mind that the patient may be asymptomatic at the time of the review, it should not be seen as a ‘snap-shot’ of the condition, more a narrative of the last 12 months, with plenty of reflective questioning of the patient.
An annual asthma review by the practice pharmacist will be, without question, person-centred. The structure should focus on the management and monitoring of the patient, empowering them to self-manage and monitor their own asthma. Treatment decisions should be made with the patient included in the decision process, with all options and alternatives discussed and documented, including taking no action.
The SIMPLES acronym—Smoking status, Inhaler technique, Monitoring, Pharmacotherapy, Lifestyle, Education, Support—is an excellent starting point when structuring an annual asthma review.22

Source: www.kingsfund.org.uk/sites/default/files/media/Anna%20Murphy_utilising%20pharmacist%20clinical%20skills.pdf
Reproduced by kind permission of Anna Murphy
Ask About Smoking
The patient’s smoking status should always be recorded in any consultation, not just at the annual review. A ‘pack year calculator’ can be used to determine a numerical value for a lifetime of tobacco exposure, both daily numbers smoked and weekly tobacco pouch use.23 The benefits of smoking cessation cannot be stressed enough to the patient, and offering Very Brief Advice (VBAs) with signposting to local specialist services is very successful.24
Take a History
Accurate history taking is imperative, not just at diagnosis but for the continued monitoring of the patient’s condition. Practice pharmacists are ideally positioned to monitor people with asthma providing they have received the appropriate training and are competent and confident—refer to the PCRS Fit to care guide for a list of required skills and competencies.25 Taking an accurate history will enable a like-for-like, year-on-year comparison to be made of the patient’s respiratory health. The Asthma Control Test (ACT™)26 and The Royal College of Physicians (RCP) ‘3 Questions’27 are both valuable tools in documenting a patient’s asthma control. If the asthma has been triggered by a seasonal pollen, it is often shrewd to set a reminder for future annual reviews 1 month before the anticipated release of the pollen.
Assess Peak Flow Results
Peak flow testing by the patient is a cornerstone in monitoring asthma.18 It can quantify what is often a qualitative expression from the patient. Key to this is establishing what a good/normal peak flow for the patient looks like, and using this to calculate threshold values in the patient’s personalised asthma action plan (PAAP). Peak flow meters are only useful when used correctly, and so the patient should never leave the consultation room without demonstrating competency in using one. Inform the patient that for quality and consistency, peak flow should be recorded twice a day (ideally at the same times), before using inhalers, and using the same meter.
There are now a number of peak flow meters designed to communicate with smartphones, either via near-field communication (NFC) technology or simply by plugging in to the headphone jack socket. The apps designed to be used with these peak flow meters can record an asthma attack or breathless episode, oral corticosteroid course, and absence from work or school.
Ensure the Patient Has a PAAP
A key recommendation of the NRAD report was the implementation of PAAPs for all patients. A PAAP is a simple, structured document to help the patient monitor and manage their asthma. It provides a visual indication, using a traffic light system, on how to maintain asthma control, how to identify a lack of control (and if so, what actions to take), and what to do after an asthma event.
The personalised aspect of the plan is vital. The patient’s trigger factors, inhaler strength and dose, and any use of a spacer device should be documented. A copy of the PAAP should be stored electronically or in the patient’s notes for future reference. For children, all parents, guardians, carers, and even teachers should be familiar with the PAAP and have a copy either on their phone or a hard copy readily available. Practitioners should be aware that co-parenting can pose unique issues, including a lack of consistency in asthma care from either parent, poor compliance, and differing trigger factors in each house.
Over three-quarters of patients who died from asthma during the NRAD review period did not have a PAAP.2 There are some barriers to implementing PAAPs, which have been addressed in the IMP2 ART study by the Asthma UK Centre for Applied Research.28
Review the Patient’s Medication
Inhaled corticosteroids are the bedrock of pharmacotherapy in asthma, and as with all inhalers they should be prescribed by brand. A target to aim for at annual review is for the patient to be symptom-free on the lowest possible dose of ICS.5–7 Inhaler technique in people with asthma, however, has not improved in over 40 years.29 With correct inhaler technique and the right inhaler, the dose of an ICS can often be reduced due to greater deposition of the dose. Yet today, with over 100 inhaler devices and combinations available to prescribe, there remain only two inhaler techniques to master: ‘slow and steady’ for pMDIs, and ‘fast and deep’ for dry powder inhalers (DPIs).
The RightBreathe app and desktop portal are invaluable in optimising inhaler use and prescribing, with links to video demonstrations of all inhalers on the UK market.30
Provide Asthma Education
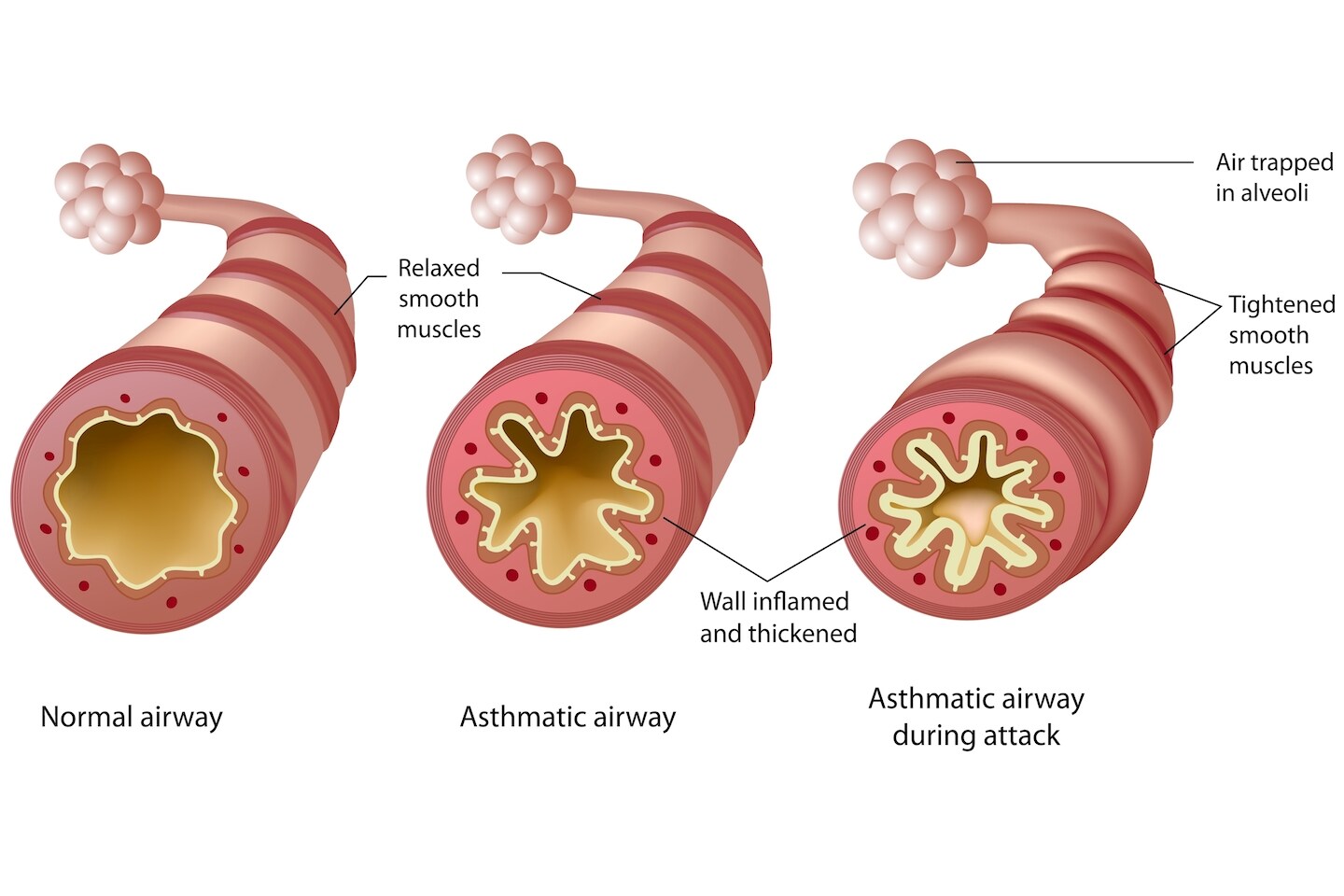
Even patients who demonstrate good inhaler technique can still forget to take their medication on a regular basis. Reminding them about the variable nature of asthma, and explaining about the underlying inflammatory condition of their lungs, is all part of the education process during the consultation.
A key concept to share with patients is that if we step up therapy after poor control, we will be looking to step back down again to the lowest ICS dose possible to maintain control. With the advent of MART (Maintenance And Reliever Therapy) licences, it is crucial that these are only prescribed to patients who can comprehend the variation in therapy after education, and obviously that they are documented in the patient’s PAAP.
Explaining that people with asthma will always have a degree of inflammation in the lung, but that it can be controlled with ICS, is fundamental to the patient’s understanding of asthma; the diagram in Figure 2 is a useful aid to convey this.
Health literacy is an important aspect of the consultation.31 As healthcare practitioners, we often undervalue the health literacy requirements of our patients. Conveying asthma management advice in small chunks, avoiding medical terminology and acronyms, and checking that patients have fully understood each chunk is crucial.
Conclusion
With prescribing budgets tighter than ever, the best inhaler on the market today is the one that the patient can use, does use, and will use. Conversely, the most expensive inhaler on the market today is the one that the patient can’t use, doesn’t use, and won’t use. Not using an inhaler, or not using it correctly, has a knock-on financial burden to the NHS as these patients invariably have more asthma attacks, present at A&E, or sadly become another statistic for a future NRAD report.
Today’s practice pharmacist is a medicines expert and brings a novel and unique skillset to the practice team in managing long-term conditions like asthma. Performing annual reviews and post-exacerbation and discharge follow ups are invaluable in helping individual patients manage and control their own asthma. With good education and inhaler technique, the patient will be in control of and able to manage their own asthma.
When patients have well-controlled asthma, optimal control can be achieved by stepping down the ICS to the lowest possible dose that still ensures good control. This is a win-win for everyone—prescribing advisers and CCGs for a lower inhaler spend, secondary care for few asthma admissions, and ultimately patients who will have a better quality of life, be less symptomatic, and will avoid becoming another NRAD statistic.
Garry McDonald
GP Practice Pharmacist and Respiratory Specialist Pharmacist, UK widePCRS Clinical Leadership Faculty, Lead Pharmacist

