Dr Steve Brown presents a range of patient case studies that illustrate different causes of a discharging ear and suitable treatment options
| Read This Article to Learn More About: |
|---|
|
The discharging ear is a common reason for patients to present to their GP, local out-of-hours centre, or to accident and emergency. Around 10% of people experience acute otitis externa at least once in their lifetime and there is an increased incidence in summer.1 Approximately 1% of all GP consultations are for acute otitis externa and 3% of cases seen in primary care are referred to secondary care.2
The example case studies presented below explore otitis externa and some of the more complex causes of a discharging ear that may be encountered in primary care, how subtle differences in symptoms can be used to differentiate between diagnoses, and how each condition should be treated—including when to refer.
Note: Some of the medicines discussed in this article currently (January 2017) do not have UK marketing authorisation for the indications mentioned. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council's Good practice in prescribing and managing medicines and devices3 for further information.
Case 1
A 21-year-old woman presents with a very painful and itchy discharging ear, and partial hearing loss. On examination the external auditory canal is swollen. She tells you that she swims regularly.
Diagnosis
Otitis externa (see Figure 1, below) can only be confirmed when you are certain that the eardrum is intact. Severe pain suggests that bacterial infection is the cause of otitis externa.
Source: Fig 7-29 Chronic Otitis Externa. Hawke Library. Dr Michael Hawke, Toronto, Canada
Treatment
Most cases of otitis externa (90%) are caused by bacteria; Pseudomonas aeruginosa and Staphylococcus aureus are the most common pathogens, but one-third of cases involve multiple bacteria.4
Earache is a common symptom of otitis externa. Many different nerves innervate the ear so earache can be a referred pain. When assessing a patient with earache where the eardrum is intact, a broad history should be taken. Structures affected can include:5
- cervical spine
- temporomandibular joint
- sinuses
- teeth
- tonsils
- post-nasal space tumours
- larynx (e.g. carcinoma).
Ciprofloxacin and ofloxacin eye drops can be used in the ear4 and although they are not licensed for this indication they are very safe with a perforated ear drum or where there is a grommet or T tube in situ.4 Aminoglycoside ear drops should be used for a maximum of 2 weeks if there is a perforated eardrum.
Patients whose symptoms are not improving may not be using ear drops properly. Advise patients to lie on their side for 2–3 minutes after inserting ear drops and to gently massage the tragus to help the drops enter the ear canal. Older patients may prefer an antibiotic ear spray, or may need help with inserting standard ear drops.
Syringing is contraindicated in the following circumstances:
- when the patient:6
- has an acute ear infection
- has a perforated eardrum or has had one previously
- has a history of ear surgery (e.g. mastoidectomy or myringoplasty)
- has a grommet in place in the ear that requires syringing
- is a young patient who is uncooperative
- it is the patient's only hearing ear.
Reasons to refer a patient to an ear, nose, and throat (ENT) clinic include:
- recurring ear infections particularly where there is debris present—microsuction is preferable to syringing for these cases
- otitis externa that does not settle with oral or topical antibiotics.
Outcome
The patient took great care to keep water out of the ear. One course of gentamycin and hydrocortisone ear drops was prescribed and the patient’s symptoms resolved after 10 days.
Case 2
A 38-year-old man, who has seborrhoeic dermatitis, presents with a painful discharging ear. He is fed up with the recurring infections, which usually respond well to antibiotic/steroid drops.
Diagnosis
For patients with recurrent otitis externa ask about, and look for, signs of eczema, seborrhoeic dermatitis, or rosacea (see Figure 2, below). Patients may have a dry itchy scalp, blepharitis, or dry skin on the face—especially around the eyelids.

Source: Fig 6-37 Chronic infective dermatitis. Hawke Library. Dr Michael Hawke, Toronto, Canada
Treatment
Once the acute infection has settled, treating these skin conditions in the external ear canal may prevent future infections. Emollients can be used in the ear as can olive oil. Steroid creams can be used to treat uninfected inflammation. Betamethasone drops (0.1%) or betamethasone scalp application (0.1%) can be used as an alternative [NB Betamethasone does not have UK marketing authorisation for the indications mentioned].
Another reason for recurring infections is using cotton buds to clean the ears. Cotton buds can push wax into, or cause damage to the skin of, the external canal providing an entry point for bacteria. Patients should be advised that wax can clear on its own as the ear canal sheds skin cells, and that using olive oil ear drops on a weekly basis can encourage the flow of wax out of the ear.
Advise patients that they should keep the ear dry and avoid putting their head underwater in the bath, as bacteria from the rest of the body can enter the ear. Patients should use ear plugs available at chemists, cotton wool covered with petroleum jelly, or moulded ear plugs (made by hearing aid companies) when washing their hair or swimming. Acetic acid drops can be used to encourage water to evaporate from the outer ear, or a hairdryer on cool can be used to dry the ear if needed.
Outcome
The patient made a concerted effort to keep his ears dry at all times and refrain from using cotton buds. He used a small amount of steroid cream if his ears became itchy and saw his GP promptly if he developed pain suggestive of infection. He needed two prescriptions for antibiotic ear drops in the subsequent 12 months for minor infections, which settled quickly. He was very pleased with his progress.
Case 3
A 72-year-old woman with diabetes, who is on methotrexate for rheumatoid arthritis, presents with a painful discharging ear. The ear canal is very swollen and the patient is in severe pain. After microsuction, granulation tissue was seen.
Diagnosis
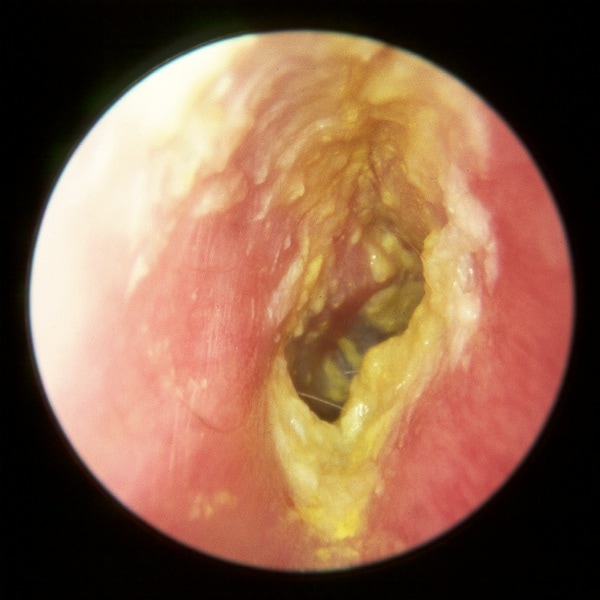
This is malignant otitis externa caused by Pseudomonas, a condition that must be recognised and treated promptly, (see Figure 3, below). A swab showing Pseudomonas does not automatically mean malignant otitis externa.

Source: Fig 7-34 Necrotizing (malignant) otitis externa. Hawke Library. Dr Michael Hawke, Toronto, Canada
People with diabetes or compromised immunity (either immunodeficient or immunosuppressed), or individuals who are frail are most at risk. The patient may present with trismus and septicaemia.
Complications of malignant otitis externa include:7
- osteomyelitis of the petrous temporal bone
- sinus and abscess formation
- meningitis
- septicaemia
- facial palsy.
Treatment
This patient needs an urgent (i.e. immediate) assessment by an ENT consultant who will most likely treat the patient with an ear wick to keep the canal open and allow antibiotic drops to soak in, and intravenous antibiotics; ciprofloxacin is the treatment of choice.4
Outcome
The patient was referred to secondary care. She had a CT scan which showed no evidence of abscess formation and no osteomyelitis. Intravenous antibiotics were prescribed for 1 week. On discharge from hospital she took oral ciprofloxacin for a further 4 weeks and then made a full recovery.
Case 4
A 22-year-old man presents with a 9-month history of a discharging ear. The discharge is present most days and is often smelly. Antibiotic drops help for only 1 or 2 days. After microsuction a scab with granulation tissue was seen in the superior part of the eardrum.
Diagnosis
The likely diagnosis of this patient is cholesteatoma (see Figure 4, below), where keratin forms a ball and burrows into the eardrum and temporal bone. It can cause hearing loss by damaging the ossicular chain, and can also lead to meningitis if it erodes towards the brain.

Source: Epidermoid cholesteatoma. Hawke Library. Dr Michael Hawke, Toronto, Canada
Cholesteatoma can cause hearing loss. Weber’s test can be used to assess for hearing loss; the tuning fork is placed in the middle of the forehead—if sound localises to the affected side it suggests a conductive hearing loss. Bone conduction is better than air conduction here. This contrasts with a unilateral sensorineural hearing loss where the sound is heard louder in the better ear. In this case air conduction is better than bone conduction.
Treatment
In this case an urgent referral to the ENT clinic is appropriate.
Outcome
The patient had a computed tomography (CT) scan to assess the extent of the cholesteatoma, and then surgery to remove it and repair the eardrum.
Case 5
A 58-year-old woman presents with a blocked and very itchy ear. She has recently needed two courses of oral antibiotics and two different types of ear drop to treat an episode of acute otitis externa. On examination, the canal is very blocked with white discharge and black flecks are visible.
Diagnosis
The most likely diagnosis is Candida and Aspergillus (see Figure 5, below) caused by her recent treatment with antibiotics. An ear swab can be used to confirm the diagnosis.

Source: Fig 7-26 Ostomycosis (Aspergillus species). Hawke Library. Dr Michael Hawke, Toronto, Canada
Treatment
This patient requires weekly microsuction for 3 weeks and treatment with clotrimazole ear solution. Microsuction is normally carried out in secondary care but specialists in primary care (with the appropriate experience and equipment) can also perform the procedure.
Clioquinol and flumetasone ear drops have antibacterial and antifungal properties and are a very good second-line treatment if a fungal infection is suspected. Warn patients that these ear drops can stain clothes (as they contain iodine).
Outcome
There was a gradual improvement in the patient’s condition as she experienced reduced aural discharge, less inflammation in the ear canal, and less itching. After 3 weeks the patient had no symptoms and the ear canal looked normal.
Conclusion
Otitis externa is a common condition in primary care. The diagnosis is usually straightforward and treatment with ear drops usually resolves the condition. Practitioners need to be aware of reasons why a patient may not improve as quickly as expected and of complications that can arise from severe infections, particularly malignant otitis externa. Referral to secondary care is appropriate for a small number of patients, either where complications have arisen, or in cases where the diagnosis is in doubt.
Dr Steve Brown

