Ruari O’Connell and Anna Prescott Describe the Role of the Clinical Practice-based Pharmacist in Managing Patients with Psoriasis
| Read This Article to Learn More About: |
|---|
This article has been developed in association with Soar Beyond Ltd.   |
Psoriasis is a common, genetically determined, chronic relapsing inflammatory and proliferative condition that affects the skin, scalp, nails, and joints.1 Psoriasis is thought to affect around 1.3–2.2% of the UK population,2 the majority of whom are managed in primary care. Although psoriasis is often described as a skin condition, it is a multisystem disorder that is associated with cardiovascular and psychological co-morbidities,1 an increased risk of mortality,3 and a significant impact on the patient’s quality of life.4
Unlike other chronic conditions, psoriasis is not part of the quality and outcomes framework (QOF) so there is no financial incentive for practices to routinely monitor psoriasis. Therefore, patients may be more likely to be identified when complications arise, rather than during a routine review where issues could have been prevented—for example, by optimising their treatment or referring for specialist advice. Psoriasis is generally a lifelong condition and the impact of suboptimal treatment can have a profound effect on the patient.5 It is therefore essential that the primary care team is equipped to manage patients living with psoriasis as effectively as they would patients with other chronic conditions.
This article reviews how clinical pharmacists working in general practice can utilise their skills to proactively manage patients with psoriasis in line with the key treatment aims highlighted in NICE Clinical Guideline 153; ‘to improve long-term disease control and quality of life for people with psoriasis.’2
Management of Patients with Psoriasis
A diagnosis of psoriasis is usually made by a GP. However, up to 60% of patients will require specialist referral at some stage2 so some patients will be seen in secondary care. There are nonetheless many opportunities for practice-based pharmacists to support patients, particularly because treatment adherence and drug monitoring are key considerations for assessing ongoing management and suitability of psoriasis medications,2 and the pharmacist is well placed to take on these aspects of care.
NICE and SIGN provide extensive guidance on how psoriasis can be managed in primary care, including:2,5
- assessment of disease severity
- assessment of cardiovascular risks
- assessment of other co-morbidities
- the impact of disease on physical, psychological, and social wellbeing
- whether the patient has psoriatic arthritis
- initiation and review of topical therapy.
Reviews of psoriasis should be offered at appropriate intervals, at least annually, to reassess severity, comorbidities, cardiovascular risk, articular symptoms, depression, and to optimise topical therapies where applicable.5
The Role of the Practice-based Pharmacist in Psoriasis
As experts in medicines, clinical pharmacists can play a key role in improving prescribing practices and medicines optimisation. This can be particularly relevant when it comes to the management of conditions that affect the skin, as well as associated co-morbidities, as they have a good understanding of the different formulations of topical therapies available. Pharmacists will be aware of the key monitoring requirements for systemic therapies that may be used to treat more severe skin conditions.
When deciding whether it is appropriate for a clinical pharmacist to take on the management of psoriasis, it is important to understand which elements of psoriasis care can be managed in primary care, and how they align with the individual pharmacist’s existing skillset.
Soar Beyond has developed a stratification tool and associated clinical system searches, based on specific prescribing patterns, to help pharmacists to easily identify patients with psoriasis who are within their scope of competence to manage (see Figure 1). Developed by an expert faculty as part of the Soar Beyond i2i network, the tool aligns what a clinical pharmacist can do with the priorities of NICE Clinical Guideline 153, Psoriasis: assessment and management, and SIGN guideline 121, Diagnosis and management of psoriasis and psoriatic arthritis in adults. It focuses on four key areas:
- psoriasis annual reviews
- adherence, appropriateness, use, and acceptability of topical treatment
- medication reconciliation and shared care
- case finding.
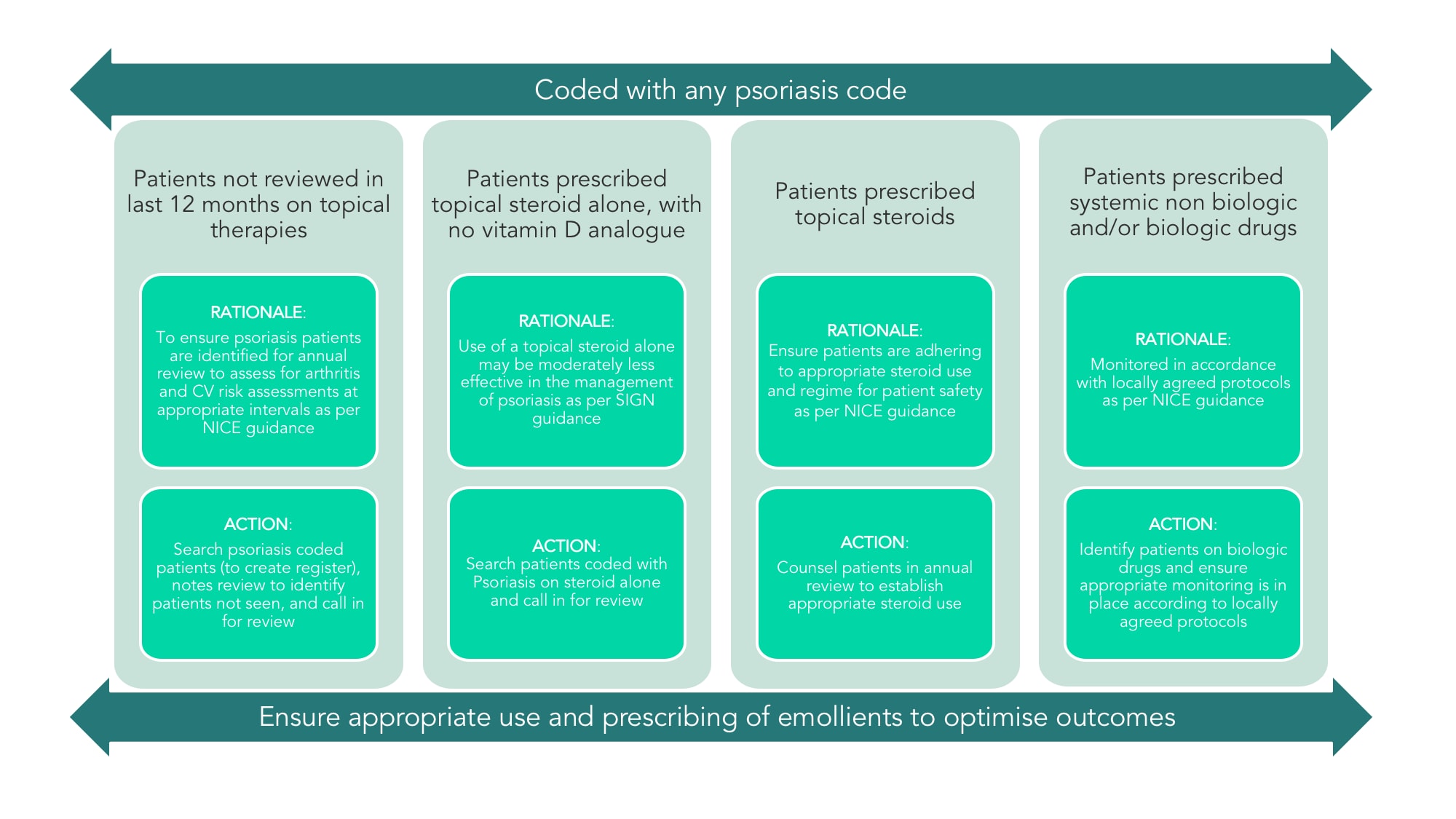
Adapted from Soar Beyond Ltd. i2i Pharmacists Network. www.i2ipharmacists.co.uk
CV=cardiovascular; SIGN=Scottish Intercollegiate Guidelines Network
Clinical pharmacists working in general practice should be able to:
- ensure that patients with psoriasis are empowered to self-manage where possible
- provide opportunities to discuss risk factors for cardiovascular co-morbidities
- offer preventative advice, and health and lifestyle information
- highlight where prompt referral to secondary care may be necessary.
Psoriasis Annual Review
Both NICE2 and SIGN5 recommend annual reviews for patients with psoriasis; however, in the authors’ experience, this does not routinely happen. If annual reviews are not regularly taking place the practice pharmacist can take an active role in setting them up. This involves creating a psoriasis register at the practice through a system search, then filtering the search to show only the patients who have not been seen for their psoriasis in the last 12 months. From the register, the pharmacist can review each patient’s notes and decide on a suitable action plan. This could form the baseline for an audit or quality improvement project aimed at encouraging learning within the multidisciplinary team and identifying gaps in patient care.
The clinical pharmacist and the practice could also consider developing a clinical system template that incorporates the elements of an annual review recommended by national guidance to ensure consistent care across the practice. This should cover:5
- documentation of severity using Dermatology Life Quality Index scoring
- screening for depression
- assessment of cardiovascular risk
- assessment of articular symptoms
- optimisation of topical therapy
- consideration of referral.
If within their scope, and depending on patient numbers, clinical pharmacists can run dedicated clinics for patients with psoriasis, or request that patients are booked in with a more suitably trained healthcare professional. The practice may also wish to create a recall system, similar to those in place for other chronic conditions, to ensure that regular reviews take place.
Treatment Options
There is a wide range of treatment options for psoriasis, the choice of which will vary depending on the type and severity of psoriasis. Options include:
- topical therapies6
- emollients
- corticosteroids
- vitamin D analogues
- coal tar
- dithranol
- tazarotene
- salicylic acid
- systemic non-biological therapies
- methotrexate6
- ciclosporin acitretin6
- apremilast7
- dimethyl fumarate8
- systemic biological therapy with monoclonal antibodies (e.g. infliximab)2
- phototherapy.6
Systemic therapies should be initiated by specialists only. Topical therapies can be initiated and continued in primary care.2
Adherence, Appropriateness, Use, and Acceptability of Topical Treatment
Evidence suggests that a lack of response to treatment can be as much to do with poor adherence as it is to do with poor efficacy.5 SIGN recommends a follow-up appointment after initiating or changing topical therapy, and that the number of treatments per day should be kept to a minimum.5 The Primary Care Dermatology Society supports the use of combination products as first-line treatment to encourage adherence.1
NICE guidance states that patients should be given practical support and advice about the use and application of topical treatments by healthcare professionals who are trained and competent in the use of topical therapies.2 Pharmacists working in a patient-facing capacity across all sectors are trained to support patients with using medications effectively and provide solutions when patients encounter problems. Medication reviews are therefore an ideal role for clinical pharmacists to take on in general practice.
Pharmacists can proactively assess treatment response, adherence, and acceptability, as well as amend regimens, and advise on appropriate use of corticosteroids (taking into account potency, length of treatment, and adverse effects). This kind of support and advice can help improve outcomes and safety for patients, while also helping to reduce waste (as well as cost). The case study in Box 1 describes how a pharmacist provided vital input in reviewing adherence, acceptability, and use of topical therapies, while demonstrating a holistic approach to care.
| Box 1: Case Study Demonstrating a Pharmacist’s Review of a Patient with Psoriasis |
|---|
Patient: 25 year-old female. Prior medical history: Psoriasis. Current medication: Prescribed a vitamin D analogue ointment, steroid ointment, steroid scalp application, and an emollient. Social history: Non-smoker, works as a childminder. Presentation: Routine appointment for contraceptive pill check, opportunistically raised an issue with psoriasis. Patient history: Diagnosed with chronic plaque psoriasis and occasional scalp psoriasis over 2 years ago. Over the last few months she has noticed gradual worsening of her scalp psoriasis, which now covers a greater area and is causing distress. Assessment of triggers: Experiences anxiety, which has worsened recently although she feels her stress levels are the same as normal. There have been no changes to usual cosmetic regimen and no new hair products. Adherence and acceptability check:
Physical examination: 5 small plaques on the scalp, one 2-pence sized plaque on the elbows, declined to show plaques on legs, but stated 2–3 on each leg, similar to size of plaques on the elbows. Pharmacist’s reflections: It is likely that this patient’s poor adherence to treatment and increased anxiety levels have led to a flare of her psoriasis. It is evident from the consultation that she is not managing her condition and perhaps does not understand what each of the medications is used for. She also has some acceptability issues relating to the products she has been prescribed. Action plan:
Follow up: Patient pleased with the new combination product, found it had been very effective at reducing the number and size of plaques and was much easier to apply. Still finding regular use of emollients difficult but trying to get into a better routine of using them. Had started to use a mindfulness app and found the ‘counted breathing’ helpful to reduce anxiety levels. |
Medicines Reconciliation and Shared Care
Patient safety relies on good communication and coordination between healthcare professionals across primary and secondary care. One of the core tasks of every practice-based clinical pharmacist, whether they are a prescriber or not, is medicines reconciliation from both discharge summaries and outpatient letters. If patients have been seen in secondary care for psoriasis, they may be discharged with medications that are considered beyond the prescribing remit of most GPs (often referred to as ‘red-list’ drugs). The prescribing of these drugs will usually remain the responsibility of the hospital or clinic. These should be noted in the patient’s clinical record as ‘hospital only’—this is particularly important when patients are being seen by multiple healthcare professionals across different sectors.
Depending on the local CCG, some ‘red-list’ drugs may be prescribed under shared care arrangements, which require monitoring or prescribing to be undertaken in primary care. The details and scope of any shared care arrangement between the GP practice and hospital must be clearly defined to ensure effective and convenient ongoing care for the patient. The clinical pharmacist can take responsibility for identifying patients taking ‘red-list’ drugs, for example by searching for patients prescribed systemic therapies, reviewing patients on the psoriasis register, and for making sure there is a robust process for receiving shared care protocols. Once patients receiving applicable treatments are identified, the clinical pharmacist can flag the records as ‘hospital only’ and help iron out any issues at transfer. They can also help the practice set up a process for proactive monitoring of patients taking red-list drugs under shared care arrangements.
Case Finding
Some patients may have a diagnosis of psoriasis that is not coded on the practice’s clinical system, which may negatively impact the care they receive if they see a clinician who is not already aware of their diagnosis. Pharmacists can search for patients prescribed topical therapies consistent with psoriasis, review their notes, and code accordingly, thus adding patients to the psoriasis register and ensuring they receive an annual review in line with national guidance. As part of this review, they can also assess the appropriateness of their treatment and identify patients who may benefit from an earlier review.
Conclusion
Psoriasis is a chronic condition that impacts more than just the skin of those affected. Psoriasis can be effectively controlled but there is variation in the ongoing management of the condition, particularly with respect to accessing specialist treatments, drug monitoring, specialist nurse support, and psychological services.9 National guidance represents one way to ensure a standardised approach to patient care, and provides primary care clinicians with appropriate advice to improve their confidence in the diagnosis, assessment, and management of psoriasis. General practices can utilise the skills of the clinical pharmacist to incorporate national guidance into the practice system, and ensure a proactive approach to patient care that will ultimately lead to improvements in the outcomes and quality of life for people living with psoriasis.
Ruari O’Connell
Senior Clinical Pharmacist
Anna Prescott
Pharmacist and Clinical Services Manager for Soar Beyond Ltd.
| Soar Beyond has developed the i2i Network to help general practices to implement, train, and develop clinical pharmacists in general practice. For more information on upcoming workshops and services, visit: www.i2ipharmacists.co.uk |

