Dr Sinan Eccles Discusses the New Recommendations from the 2019 BTS/SIGN Asthma Guideline, Including Updated Advice About Monitoring Asthma
| Read This Article to Learn More About: |
|---|
Find key points, useful resources, and implementation actions for STPs and ICSs at the end of this article |
In the UK, 1 in 12 adults and 1 in 11 children are receiving treatment for asthma: a total of 5.4 million people.1 The NHS spends approximately £1 billion annually on treating and caring for people with asthma, and in 2016–2017 asthma was responsible for over 77,000 hospital admissions and almost 1500 deaths in the UK.1
The British Thoracic Society/Scottish Intercollegiate Guidelines Network (BTS/SIGN) British guideline on the management of asthma2 has offered guidance on asthma care over the past two decades, since the two organisations first jointly produced an evidence-based guideline in 2003. The guideline has been strengthened over time through collaboration with other groups, including Asthma UK, the Royal College of Physicians (RCP), and the Primary Care Respiratory Society UK.
In 2017, NICE published guidance on Asthma: diagnosis, monitoring and chronic management.3 There are significant differences in the scope, methodology, and some recommendations between the BTS/SIGN and NICE guidelines, which have been discussed in detail elsewhere.4 The BTS/SIGN guideline is a ‘living’ guideline; key sections are regularly updated to reflect new evidence. The most recent update, SIGN 158, was published in July 2019.2 There are major revisions relevant to primary care in the 2019 version, particularly in the sections on monitoring asthma, supported self-management, and pharmacological management.
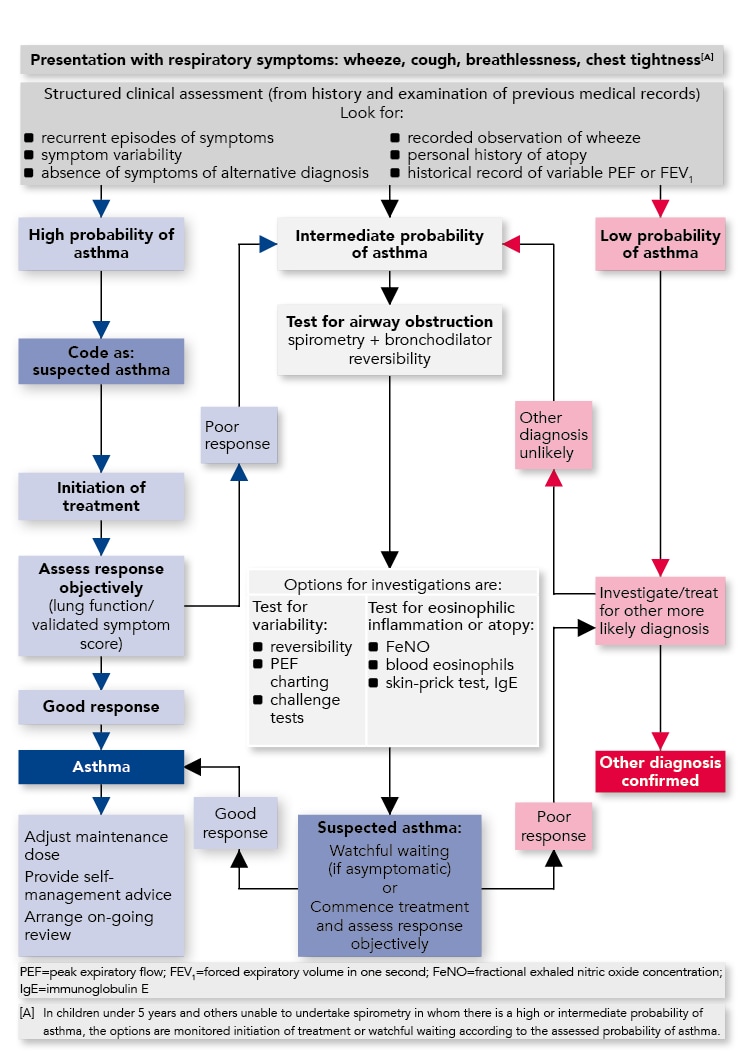
Diagnosis
Recommendations on the diagnosis of asthma remain unchanged from the 2016 version of the BTS/SIGN guideline. Asthma is a clinical diagnosis with no single diagnostic test, so a structured approach to diagnosis is required. This includes a structured clinical assessment to determine the likelihood of asthma, supported by objective testing for variable airflow obstruction and airway inflammation.
Clinical response to a monitored trial of treatment with an inhaled corticosteroid (ICS) can help confirm or refute the diagnosis.
The recommended diagnostic pathway is summarised in Figure 1. An in-depth commentary on diagnosing asthma in line with BTS/SIGN guidance has previously been published in Guidelines in Practice.5
British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. SIGN 158, updated 2019. Available at www.sign.ac.uk/our-guidelines/british-guideline-on-the-management-of-asthma:
Monitoring and Reviewing Asthma
An asthma review should be undertaken at least annually by a healthcare professional with appropriate training. Reviews can take place in primary or secondary care depending on clinical need and local service arrangements.2 Identifying individuals with poor symptom control and/or a high risk of future attacks allows targeting of care with medication, lifestyle measures (e.g. smoking cessation support), a personalised asthma action plan (PAAP), and more frequent review. The core components of an asthma review are summarised in Table 1. Use of a paper or electronic proforma can help ensure all important aspects are covered during a structured asthma review.
Table 1: Components of an Asthma Review2
| Parameters | Suggested Assessment |
|---|---|
| Current symptom control |
|
| Future risk of attacks |
|
| Tests/investigations |
|
| Management |
|
| Supported self-management |
|
SABA=short-acting beta2 - agonist; ICS=inhaled corticosteroid; PEF=peak expiratory flow Adapted from British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. SIGN 158, updated 2019. Available at: www.sign.ac.uk/our-guidelines/british-guideline-on-the-management-of-asthma. Reproduced with permission. | |
Current Symptom Control
When asking about current symptom control, direct questions (such as ‘How often do you use your reliever inhaler?’) are more likely to yield useful information than more general, open questions (such as ‘How is your asthma control?’). The RCP ‘three questions’6 are a useful starting point for discussion:
- have you had difficulty sleeping in the last week because of your asthma (including cough)?
- have you had your usual asthma symptoms during the day (cough, wheeze, chest tightness, or breathlessness)?
- has your asthma interfered with your usual activities (e.g. housework/school, etc.) in the last week?
If the answer to all three questions is ‘No’, asthma control is likely to be good. A ‘Yes’ to one or more questions should prompt further assessment. This is best achieved by using a validated questionnaire such as the Asthma Control Questionnaire (ACQ), Asthma Control Test (ACT), or Childhood Asthma Control Test (C-ACT).
Children should be asked about their own symptoms, whenever this is practicable; relying solely on what parents or guardians report can sometimes be misleading.2
Predicting Future Risk of Asthma Attacks
In adults, the strongest predictor of future asthma attacks is a previous history of asthma attacks. Poor symptom control, as measured by a validated symptom questionnaire, is associated with a moderately increased risk of future attacks.2 Excessive short-acting beta2 -agonist (SABA) reliever inhaler use is also associated with a moderately increased risk of future attacks,2 and was identified as a marker for increased risk of asthma death in the RCP National review of asthma deaths (NRAD).6 Patients who are prescribed more than 12 SABA inhalers per year should be identified and their management reviewed. This information can often be obtained from electronic patient records. Older age, female sex, reduced lung function, obesity, smoking, and depression are all associated with a slightly increased risk of future asthma attacks in adults.2
In children aged 5–12 years, a history of previous asthma attacks and persistent asthma symptoms are associated with a greatly increased risk of future asthma attacks. The ratio of prescriptions of controller to reliever inhalers is a useful marker in children: if more than 50% of prescriptions have been for reliever inhalers, this is associated with a moderately increased risk of future attacks. Co-morbid atopic/allergic disease and vitamin D deficiency are also associated with a moderately increased risk of future attacks. Social factors such as being from a low-income family (moderate increase), exposure to environmental tobacco smoke (slight increase), and low parental education (slight increase) are markers of increased risk of future attacks, as are younger age and obesity (both slight increase).2
There is limited evidence available to guide risk prediction of future attacks in pre-school children.2
People with severe asthma will usually be under specialist follow up to guide their management. Nevertheless, previous attacks, very poor symptom control, greater SABA use, and lower lung function are again markers of an increased risk of future attacks.2 A raised fraction of exhaled nitric oxide (FeNO) is also predictive of future attacks in this group, but routine use of FeNO testing to monitor asthma is not recommended outside specialist asthma clinics.2
Clinicians should target care to people with poor current control and/or a high risk of future attacks, including tailoring frequency of review, optimising pharmacological therapy, personalising supported self-management, and considering referral to specialist care where appropriate.
Tests and Investigations
A measure of lung function should form part of a structured asthma review. Spirometry is reproducible, can give a measure of airflow obstruction, and can be used in children as young as 5 years of age.2 Reduced lung function is associated with an increased risk of attacks, particularly in adults, and some adults have an accelerated decline in lung function over time.2 In this subgroup, it is worth revisiting the diagnosis to ensure it is correct. Further research is needed to identify risk factors and develop treatment strategies for these patients.2 Peak expiratory flow (PEF) rate can also be used as a measure of airflow obstruction and is easier to perform than spirometry.
In children, growth (height and weight centile) can also contribute to this section of a structured asthma review.
Management
Review of management is not limited to a review of medication. Many patients do not complete the necessary steps to use their inhalers successfully,7 and assessment and reinforcement of inhaler technique forms a vital part of an asthma review. Information on inhaler technique, including instructional videos, is available for free online, including from www.asthma.org.uk/advice/inhaler-videos.8 Equally important is an assessment of adherence to treatment, which can be self-reported through an open discussion with the patient, and by checking prescription refill frequency since the last review.2
Non-pharmacological management includes avoidance of known triggers of an individual’s asthma where possible,2 particularly smoking and second-hand smoke exposure. While house dust mite sensitisation is a common trigger, methods to reduce house dust mite levels in the home should not routinely be recommended by healthcare professionals.2 Weight-loss advice and interventions should be considered for overweight and obese adults and children as, in addition to the wider health benefits, excess weight is associated with worse asthma control and an increased risk of future attacks.2
Breathing exercise programmes can help improve quality of life and improve symptoms in adults with incomplete asthma control.9 These are usually taught by physiotherapists, although a growing array of audiovisual resources are becoming available online. It should be made clear to patients that these programmes are an adjunct to, not a substitute for, their usual asthma medication.
Review of pharmacological management (discussed in more detail later in this article) should include an assessment of whether the current treatment is adequate, or whether an increase or decrease in treatment would be appropriate. Consideration of co-morbidities and polypharmacy is also important.
Supported Self-management
A self-management programme includes education regarding asthma and its treatment, and provision of a written personalised asthma action plan (PAAP)—versions for adults and children are available from many sources (including from www.asthma.org.uk/advice/manage-your-asthma/action-plan, which also provides advice on how to complete a PAAP).10 A PAAP gives specific advice on recognising loss of asthma control and exacerbations, and actions to be taken based on different thresholds of symptoms and/or reduction in PEF, or by symptoms alone in younger children. The PAAP could also include action points on seeking emergency help, starting a ‘rescue pack’ of oral steroid tablets, or temporarily increasing the dose of ICS.2
Patients who use a single fixed-dose ICS with long-acting beta2 -agonist (LABA) combination inhaler for both maintenance and reliever therapy (MART) should have their PAAP tailored to reflect this regimen. For those not on a MART regimen, quadrupling the dose of ICS at the onset of an asthma attack and for up to 14 days can help reduce the risk of needing oral steroids. This approach may be less effective in patients who are already highly adherent to their maintenance treatment, and the risks and benefits of this approach should be weighed up in patients who are already on a high dose of ICS. For patients who use a combination inhaler containing ICS and a LABA, increasing the dose of ICS may be best achieved by adding a single ICS inhaler.2
Pharmacological Management
An up-to-date evidence review on the pharmacological management of asthma was undertaken for the 2019 version of the BTS/SIGN guideline. The updated NICE asthma guideline published in 2017, gave some recommendations that conflicted with previous editions of the BTS/SIGN guideline. NICE recommends a SABA as first-line treatment,3 whereas BTS/SIGN recommends that patients with a diagnosis of asthma should commence a regular preventer medication, usually with an ICS inhaler.2 Asthma is an inflammatory condition, and treatment with bronchodilators alone will not address the underlying airway inflammation that causes the disease. Underuse of preventer medication was identified as an important risk factor for asthma death in the NRAD report.6
Prior to the 2016 BTS/SIGN guideline update, the steps in treatment were numbered 1 to 5, with ‘SABA as required’ as step 1, ‘low dose ICS’ as step 2 and so on. There was concern that the removal of what was previously step 1 would cause confusion, so the guideline moved to naming rather than numbering the steps. The renaming itself has caused some confusion while healthcare professionals adjusted to the changes. In the 2019 update, the steps have been simplified, with a reduced number of suggestions at certain steps. The recommended steps of treatment are summarised in Figures 2 and 3.
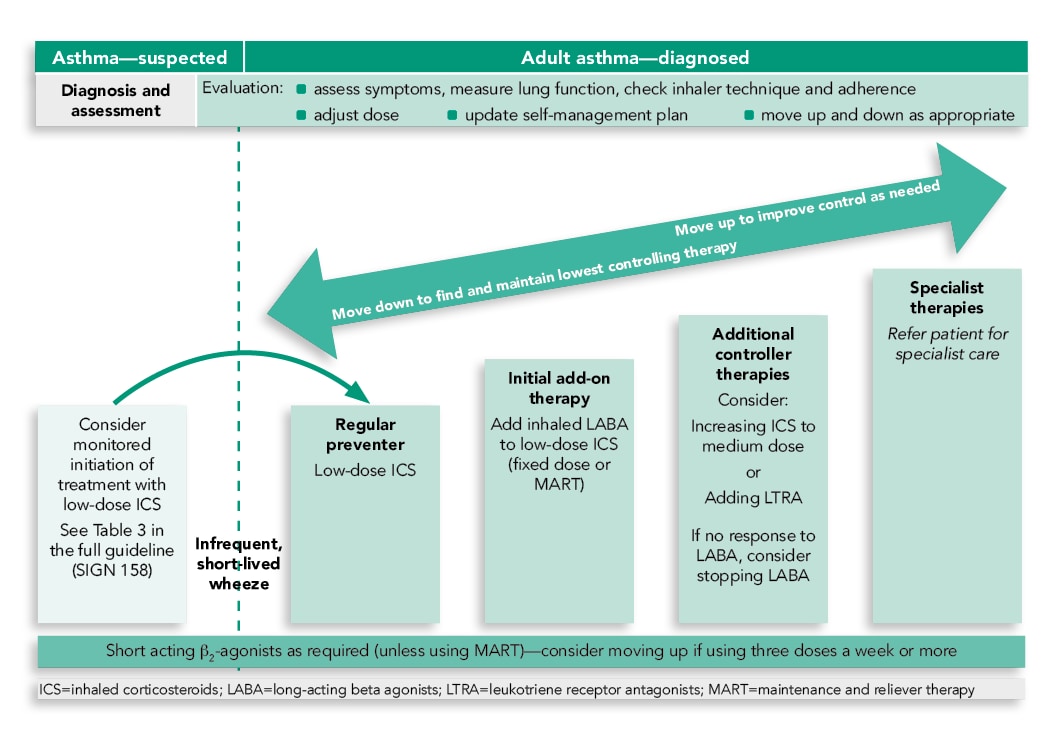
British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. SIGN 158, updated 2019. Available at: www.sign.ac.uk/our-guidelines/british-guideline-on-the-management-of-asthma
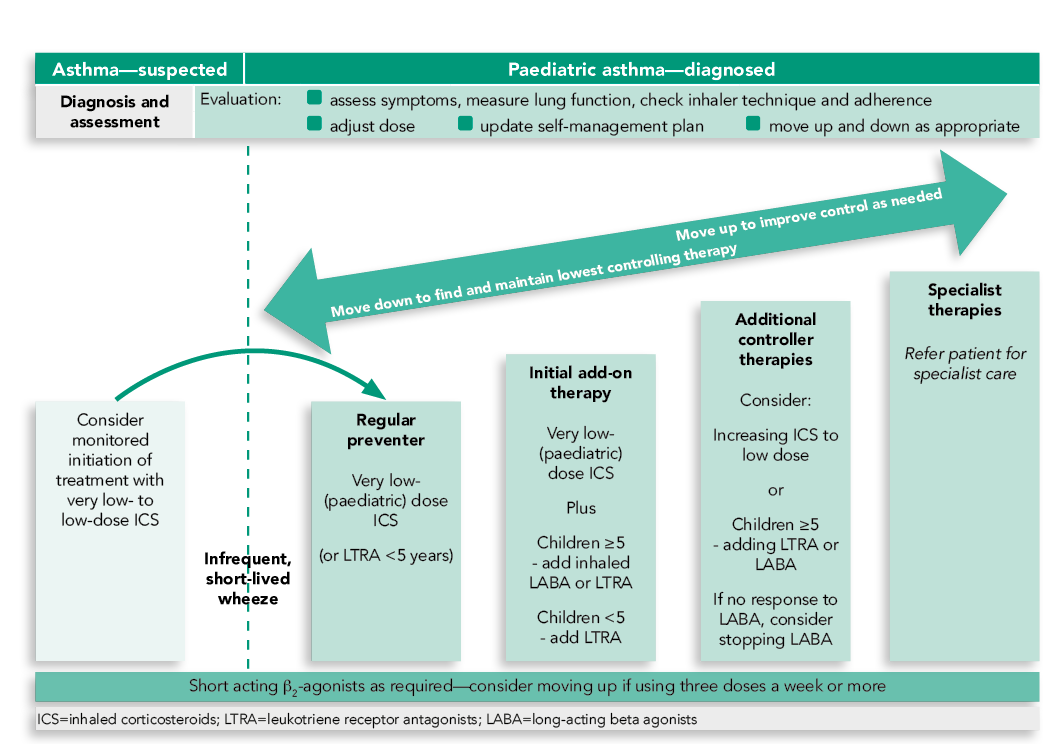
British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. SIGN 158, updated 2019. Available at: www.sign.ac.uk/our-guidelines/british-guideline-on-the-management-of-asthma
A key difference between the 2016 BTS/SIGN guideline and the 2017 NICE guideline was the initial add-on therapy if asthma in adults is uncontrolled with a low-dose ICS. BTS/SIGN reviewed the most up-to-date evidence and continue to recommend addition of a LABA to low-dose ICS in this situation, followed by increasing the dose of ICS or adding a leukotriene-receptor antagonist (LTRA) as the next step.2 Inhaler technique and medication adherence should be reviewed every time a change in treatment is considered, and any issues should be addressed before trialling a step up in medication.
BTS/SIGN now recommends that if asthma is still uncontrolled despite additional controller therapies, or there is a poor response to monitored initiation of asthma treatment in children, referral to a specialist is warranted.2 A review of the management of severe asthma is beyond the scope of this article, but briefly, a specialist review will allow re-assessment and confirmation of the diagnosis (many conditions can mimic ‘difficult’ asthma), further assessment of factors such as concordance with medication, and ‘phenotyping’ to determine what ‘type’ of asthma a patient has. This includes measures of inflammation, atopy, airflow obstruction, and other factors. The range of specialist therapies available is expanding, ranging from simple interventions such as long-acting muscarinic antagonist inhalers, monoclonal antibody treatments that target eosinophilic inflammation or atopic pathways, and highly specialist procedures such as bronchial thermoplasty.
Conclusion
This article summarises some of the key messages of the 2019 update of the BTS/SIGN British guideline on the management of asthma,2 including guidance on a structured approach to diagnosis, an in-depth discussion on the core components of an asthma review, and the simplified steps of asthma management. Implementing the guidance may require a change in practice to ensure that asthma reviews are structured to cover all the important aspects. Use of an electronic or written proforma could help facilitate this.
The other major challenge for primary care is how best to manage patients in the face of conflicting national guidelines. An agreement has been reached between BTS, SIGN, and NICE that they will jointly produce future UK guidance on chronic asthma, which should reduce the confusion for healthcare providers caused by conflict between the current sets of guidelines.
Dr Sinan Eccles
Consultant Respiratory Physician, Royal Glamorgan Hospital. Member of the SIGN 158 guideline development group
| Key Points |
|---|
RCP=Royal College of Physicians SABA=short-acting beta2 -agonist; LABA=long-acting beta2-agonist; ICS=inhaled corticosteroid |
| Useful Resources |
|---|
|
| Implementation Actions for STPs and ICSs |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved with implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
STP=sustainability and transformation partnership; ICS=integrated care system; BTS=British Thoracic Society; SIGN=Scottish Intercollegiate Guidelines Network; QOF=quality and outcomes framework |

