Dr Louise Warburton Reviews the Latest Recommendations from NICE on the Management of Rheumatoid Arthritis in Adults
| Read This Article to Learn More About: |
|---|
Find key points and implementation actions for STPs and ICSs at the end of this article |
Rheumatoid arthritis (RA) is a disabling auto-immune disease, which affects about 1% of the UK population. It causes joint pain and swelling due to synovitis and, if left untreated, can cause long-term joint destruction and disability. The disease is more common in people who smoke. Prevalence is higher in women; about three times as many women are affected as men.1 It can occur at any age but onset typically occurs between the ages of 40 and 60 years. People with early symptoms of RA often present to primary care. Symptoms can be difficult to spot if they do not cause the classical symmetrical arthritis of the small joints of the hands and feet.
In February 2009, NICE published the first clinical guideline (CG) on Rheumatoid arthritis in adults: management (CG79), with the aim of improving early detection of rheumatoid arthritis (RA) in primary care and ensuring prompt referral to specialist care. NICE CG79 recommended that, once in specialist care, patients received early treatment with disease-modifying anti-rheumatic drugs (DMARDs).
Later in 2009, the National Audit Office reported that early aggressive treatment of RA was cost-effective, but also acknowledged that there was significant geographical variation in RA care across the UK.2
In 2013 NICE published Quality Standard (QS) 33 on Rheumatoid arthritis in over 16s, which supported early referral and treatment, through the following quality statements:3
- Statement 1: people with suspected persistent synovitis affecting the small joints of the hands or feet, or more than one joint, are referred to a rheumatology service within 3 working days of presentation
- Statement 2: people with suspected persistent synovitis are assessed in a rheumatology service within 3 weeks of referral
- Statement 3: people with newly diagnosed rheumatoid arthritis are offered short-term glucocorticoids and a combination of disease-modifying anti-rheumatic drugs by a rheumatology service within 6 weeks of referral.*
*This quality statement was amended in 2018. Please read the text below and refer to NICE QS33 for the updated quality statements.
Since publication of both NICE CG79 and NICE QS33, the British Society for Rheumatology has performed two national audits to assess the implementation of the guidance; the first took place in 20144 and the second in 2015.5 The results indicate that, despite the NICE guidance, there are still delays in the recognition of inflammatory arthritis in primary care and referral to specialist care.4,5
The 2015 audit revealed that:5
- only 20% of patients were referred to a rheumatology service within 3 working days of diagnosis and, on average, the referral took about 20 days
- nationally, just 37% of patients were seen within 3 weeks of referral
- about two-thirds of patients referred with new-onset RA started a combination of steroids and DMARDs within 6 weeks of referral.
These factors were taken into consideration when developing NICE Guideline (NG) 100 on Rheumatoid arthritis in adults: management,6 and updates to NICE QS33,3 published in July 2018. NICE Guideline 100 replaces NICE CG79, and includes several updated recommendations based on new evidence. This article discusses the new and updated recommendations in NG100 that are relevant to primary care clinicians.
Referral
The most important recommendations for GPs to be aware of is that people with suspected RA should be referred urgently to a specialist:6
‘Refer for specialist opinion any adult with suspected persistent synovitis of undetermined cause. Refer urgently (even with a normal acute-phase response, negative anti-cyclic citrullinated peptide [CCP] antibodies or rheumatoid factor) if any of the following apply:
- the small joints of the hands or feet are affected
- more than one joint is affected
- there has been a delay of 3 months or longer between onset of symptoms and seeking medical advice.’
The recommendation was amended with the aim of preventing delays in the referral of people with new-onset RA who have normal blood findings. It has been recognised that such cases experience significant delays in referral.7
Approximately 20% of patients newly diagnosed with RA will be seronegative for rheumatoid factor and anti-CCP antibodies; they will still have active RA and should be referred promptly. However, research has shown that these patients are not rapidly referred, and sometimes wait months (or even years) for referral, often with very active disease.8
Synovitis is defined as soft-tissue joint swelling.6 In the author’s experience, urgent referral is only necessary for patients with joint pain and swelling. Many people have joint pain without swelling, which can be due to causes such as osteoarthritis and fibromyalgia.9 In such cases, referral to an interface service, physiotherapy, or a pain clinic may be required but urgent referral to a rheumatologist is not necessary.
See Figure 1 for an algorithm describing referral, diagnosis, and investigations for rheumatoid arthritis.10
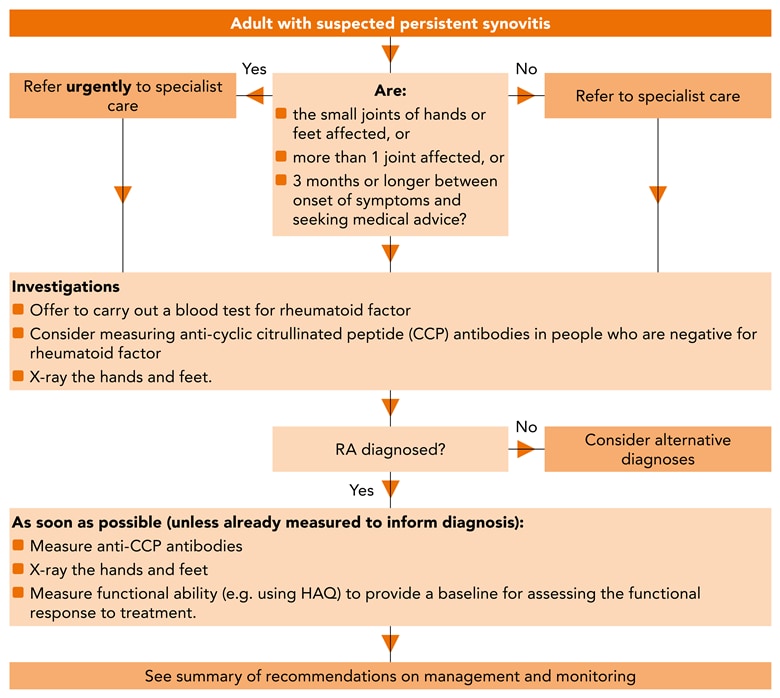
© NICE 2018 Rheumatoid arthritis in adults: management. Rheumatoid arthritis: referral, diagnosis and investigations algorithm. Available from: www.nice.org.uk/ng100 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication. See www.nice.org.uk/re-using-our-content/uk-open-content-licence for further details.
RA=rheumatoid arthritis; CCP=cyclic citrullinated peptide; HAQ=health assessment questionnaire
Investigations in Primary Care
The delay in referral caused by negative investigations was taken into account in the writing of the updated recommendations on investigations; NG100 recommends that if investigations are ordered in primary care, they should not delay referral for specialist opinion.6
The Guideline Development Group (GDG) was mindful that once a referral is received in specialist care, the triage process for the referral is aided by access to the results of recent investigations, such as tests for rheumatoid factor and anti-CCP antibodies. The GDG did not want referrals to be delayed while awaiting results or to prevent the referral of symptomatic patients with normal results. The investigations for diagnosis of RA are listed in Box 1.
| Box 1: Investigations for Diagnosis6 |
|---|
RA=rheumatoid arthritis; CCP=cyclic citrullinated peptide © NICE 2018 Rheumatoid arthritis in adults: management. Available from: www.nice.org.uk/ng100 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication. Seewww.nice.org.uk/re-using-our-content/uk-open-content-licence for further details. |
Blood tests, such as the assessment of anti-CCP antibodies, can be initiated in primary care. Rheumatoid factor is not particularly sensitive or specific for diagnosing RA. Anti-CCP antibodies are far more specific for RA (about 80% specific) and can help in the diagnosis.11
More information about anti-CCP antibodies was added to NG100 to reinforce the message that patients with anti-CCP-positive disease tend to progress more rapidly and develop erosive RA, and potentially more joint damage.6 Patients must also be vigilant for signs of disease progression and seek help if this happens.6
Treat-to-Target Strategy
Since the 2009 guideline was produced, more evidence has become available on the effectiveness of a ‘treat-to-target’ regimen.12 Treat-to-target regimens involve careful and frequent monitoring of patients after diagnosis and treatment initiation with DMARDs, and escalation of treatment to bring the disease under rapid control.
Regular disease-activity scoring is recommended to measure and accurately record the level of disease activity:6 this allows the drug treatment to be titrated up to control inflammation. The treat-to-target approach has been shown to bring the disease under effective control, reduce joint damage, and improve long-term outcomes.12
The aim of RA treatment is to achieve the lowest disease activity possible or, if feasible, total remission, because this improves long-term outcomes. Prior to publication of the 2009 guideline, it was common practice to administer a single DMARD and assess the patient again a minimum of 6 months later. There was no escalation of treatment for 6 months, and this allowed considerable joint damage to occur in some patients. The treat-to-target regimen has been one of the most successful innovations in rheumatology in the past decade. Recommendations from NG100 on the target-to-treat strategy are listed in Box 2.
| Box 2: The Treat-to-Target Strategy6 |
|---|
RA=rheumatoid arthritis; CCP=cyclic citrullinated peptide; CRP=C-reactive protein; DAS28=Disease Activity Score 28 © NICE 2018 Rheumatoid arthritis in adults: management. Available from: www.nice.org.uk/ng100 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication. See www.nice.org.uk/re-using-our-content/uk-open-content-licence for further details. |
Pharmaceutical Treatment
NICE CG79 recommended a combination of DMARDs for first-line treatment of RA. More recent evidence does not support the use of combination DMARDs, and many rheumatologists are not keen to use combinations because of their more frequent adverse effects and worse tolerability.6 Therefore, NG100 has reverted to recommending conventional DMARD monotherapy (using oral methotrexate, leflunomide, or sulfasalazine) as first-line treatment. Monotherapy should be initiated as soon as possible and ideally within 3 months of onset of persistent symptoms.6
NICE recommends that hydroxychloroquine should be considered for first-line treatment as an alternative to oral methotrexate, leflunomide, or sulfasalazine for mild RA or palindromic disease.6
NICE also recommends that short-term bridging therapy with glucocorticoids (oral, intramuscular, or intra-articular) should be considered to bring the disease under rapid control while waiting for the DMARD to take effect, which can take 4–6 weeks.6 Step-up therapy with additional DMARDs is recommended for patients whose disease does not come under rapid control with a single DMARD. This allows combination DMARDs to be used, but only when required.6
Symptom Control
The use of non-steroidal anti-inflammatory drugs (NSAIDs, including traditional or cyclo-oxygenase [COX] II-inhibitors) should be considered when control of pain or stiffness is inadequate.6 When oral NSAIDs are used to treat the symptoms of RA:6
- offer the lowest effective dose for the shortest possible time
- offer a proton pump inhibitor alongside the NSAID and
- review risk factors for adverse events regularly.
It is worth remembering that NSAIDs can be very effective at controlling symptoms while acute inflammation is being brought under control, and therefore they should not be overlooked.5,13 There is a tendency for GPs and patients to worry about NSAIDs, but they do have a useful function in the short term.
Monitoring
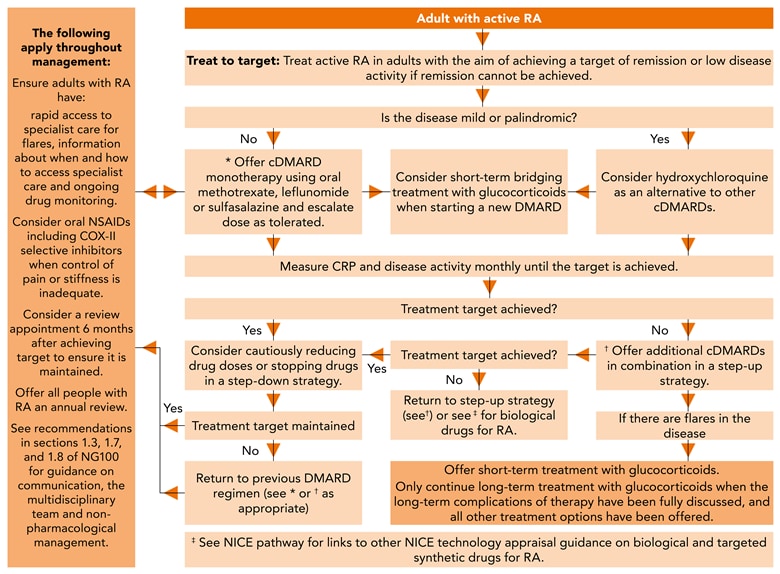
The recommendations around monitoring have been updated to further emphasise the need for access to specialist advice when the patient has a flare of disease activity. Patients should be provided with information about how and when to access specialist care. Drug monitoring should be ongoing, and is usually managed under shared-care arrangements between primary care and the specialist team once the patient is stable. An overview of the management and monitoring of people with rheumatoid arthritis is provided by the algorithm in Figure 2.14
See recommendations in section 1.10 of NG100 for guidance on timing and referral for surgery.
© NICE 2018 Rheumatoid arthritis in adults: management. Rheumatoid arthritis: management and monitoring algorithm. Available from: www.nice.org.uk/ng100 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication. See www.nice.org.uk/re-using-our-content/uk-open-content-licence for further details.
RA=rheumatoid arthritis; cDMARD=conventional disease-modifying anti-rheumatic drug; NSAID=non-steroidal anti-inflammatory drug; COX-II=cyclo-oxygenase 2; NG=NICE Guideline; CCP=cyclic citrullinated peptide
Review
Once remission (or low disease activity) is achieved, a review after 6 months is recommended, with annual reviews thereafter.6
All adults with RA, including those who have achieved the treatment target, should be offered an annual review to:6
- assess disease activity, damage, and functional ability (for example, using the Health Assessment Questionnaire)
- check for the development of co-morbidities, such as hypertension, ischaemic heart disease, osteoporosis, and depression
- assess symptoms that suggest complications, such as vasculitis and disease of the cervical spine, lungs, or eyes
- organise appropriate cross referral within the multidisciplinary team
- assess the need for referral for surgery
- assess the effect of the disease on a person’s life.
The recommendations around the annual review have been updated to further define what should be happening at this important appointment. In the 2009 guideline, it was unclear whether the annual review should be conducted in primary or specialist care. The new guideline outlines what should be evaluated at the annual review and what should be discussed with the patient. This would mostly likely occur in specialist or interface care, because primary care clinicians may not have sufficient specialist knowledge to accurately assess disease activity.
Once the disease is under control, step-down therapy is recommended. This involves a cautious reduction from two DMARDs to one, followed by a decrease in dose until the minimum dose necessary to control disease activity is achieved.6
In addition to the guideline, a helpful referral pathway with embedded referral advice is now available on the NICE website (see: pathways.nice.org.uk/rheumatoid-arthritis).
Summary
NICE Guideline 100 on RA builds upon the concepts of early referral and treatment present in the original 2009 guideline. Updated advice is given on what investigations should be undertaken in primary care and when patients should be referred. The revised recommendations emphasise that referral should not be delayed while awaiting results of investigations. Furthermore, the guideline advises that negative investigations do not mean that a patient does not have inflammatory arthritis. After diagnosis, first-line treatment with a single DMARD is recommended, with bridging steroids to bring the disease under swift control.
Dr Louise Warburton
GP and GPwSI in rheumatology
Member of the guideline development group for NG100
Associate Medical Director, Shropshire Community Trust
| Key Points |
|---|
RA=rheumatoid arthritis; NG=NICE Guideline; DMARDs=disease-modifying anti-rheumatic drugs |
| Implementation Actions |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved with implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
CCP=cyclic citrullinated peptide; QOF=quality and outcomes framework; RA=rheumatoid arthritis; DMARDs=disease-modifying anti-rheumatic drugs |

