Dr Emma Nash Discusses the Role of Primary Care in Assessing and Monitoring Patients who Present with Symptoms and Risk Factors for Eating Disorders
| Read This Article to Learn More About: |
|---|
|
This article examines the different types of eating disorder and their presentation, and offers some tips on recognition in primary care. Eating disorders affect at least 700,000 people in the UK, although the numbers are likely to be significantly higher than this because many individuals do not present to health services.3 NICE treatment recommendations state that general practice should refer all people with a suspected eating disorder to an age-appropriate eating disorder service for assessment.4,5 However, the waiting times for these services have increased considerably, with three times the number of children and young people waiting for assessment at the end of 2020 compared with the end of 2019.6 With this delay in assessment, responsibility is falling on GPs to provide holding measures and, along with charitable organisations, to do the best they can for patients during this time. This article discusses what GPs can do while their patients are waiting for assessment, particularly in terms of identifying sick patients who need urgent specialist input.
Anorexia Nervosa
Although anorexia nervosa is the least common eating disorder worldwide,7 it has the highest death rate of any mental health condition.3 Managing patients with anorexia nervosa and their physical health in primary care can be quite daunting, but there are tools available to support this. Before making the diagnosis of anorexia nervosa, it is important to establish that there is no organic pathology or social disadvantage that is causing the low weight. Physical causes include:8
- malabsorption (for example, because of coeliac disease, inflammatory bowel disease, or peptic ulceration)
- cancer of any location
- misuse of drugs or alcohol
- infection (especially occult infection like HIV, tuberculosis, or infectious mononucleosis, or a parasitic infection)
- autoimmune conditions
- endocrinological conditions (for example, diabetes mellitus [typically type 1 if weight loss is rapid], hyperthyroidism, or adrenal insufficiency).
Enquiring about availability of food is also essential: in 2019–2020, 9.2 million people in the UK—14% of the population—were living in absolute poverty.10 Making assumptions that this doesn’t apply can result in delayed help and unnecessary investigation.
Patients with anorexia nervosa have a significantly low body weight, with a body mass index (BMI) of less than 18.5 kg/m2 (or a BMI-for-age under the fifth percentile in children and adolescents), or rapid weight loss of more than 20% of their body weight within a 6-month period.1 In addition, there are behaviours that prevent gain of weight and preoccupation with a distorted perception of their weight. The individual may not see themselves as being underweight, and may even believe that they are overweight.1 Measures to avoid weight gain may include restricting food intake, purging, or creating a calorie deficit by excessive activity.1 The prospect of weight gain is often met with intense psychological distress.
Holistically Assess Individuals with Suspected Anorexia Nervosa
Of course, individuals with anorexia nervosa may not present to primary care with concerns regarding weight; many secondary clinical features may prompt someone to seek consultation. These can include amenorrhoea, tiredness, feeling cold, depression, anxiety, palpitations, reflux, and skin and hair changes.11,12 Other clinical findings, such as low blood pressure, bradycardia, or hypothermia, may also be picked up elsewhere and flagged to the GP for review.11 Obtaining an extensive history can be valuable—mentions of social avoidance in situations involving food, observed changes in eating behaviour or dress (for example, baggy clothes to hide weight loss) and remarks about excessive time spent in the toilet (for example, self-induced vomiting or laxative misuse) or excessive exercising can all provide useful clues. Screening tools exist to help in the diagnosis of eating disorders; one such resource is the SCOFF tool, which consists of five questions designed to investigate the patient’s relationship with food, eating habits, perception of their weight, and patterns of weight loss.13 Each affirmative answer scores one point; a score of two or more indicates a likely case of anorexia or bulimia.13 However, diagnostic tools alone should not be used as a basis for exclusion of illness.
Other factors can also be considered when putting together the picture of a potential eating disorder. There is often a trigger for the onset of the disorder, such as a stressful life event; it is also more common in those with a history of anxiety disorders or those who have expressed obsessional traits in childhood.2 Individuals in certain occupations are more likely to develop the disorder, in particular those with a media presence or elite athletes.2 Other mental health conditions, and alcohol and drug misuse, may also be present in patients with anorexia.2 It is important to ask about bullying, including via the internet and social media, particularly in children and young people.
Refer Individuals to Eating Disorder Services and Continue Monitoring in Primary Care
Once a possible diagnosis of anorexia nervosa—or indeed any other eating disorder—has been established, the individual needs to be referred to specialist eating disorder services.4,5 Early input is crucial. However, there are also interventions and signposting that can take place from primary care. The charity Beat offers a multitude of information, resources, and support for patients and families, and is a good place to start.14
If there is a coexisting mental health pathology, this can be addressed in primary care, with psychological interventions for depression and anxiety. However, ensure that physical state is assessed before starting any medication, because side effects, such as electrolyte imbalance, hypotension, and QT interval prolongation, are more likely in patients with anorexia and malnutrition.5 Explicitly asking about suicidal ideation is essential, as 20% of deaths in anorexia nervosa are due to suicide.3
Be Aware of ‘Red Flags’
A physical assessment needs to be carried out at the point of referral and, depending on the level of concern, may need to be repeated until the patient is seen by an eating disorder service. Depending on local arrangements, GPs may continue monitoring even when the patient is under the care of an eating disorders service. However, normal findings do not exclude a diagnosis of anorexia nervosa.
A number of assessments need to be made, and the red-flag signs for severe illness watched out for. This includes signs of malnutrition, as well as concerning physical symptoms or test results:15
- a BMI of less than 13 kg/m2; or, for people under 18 years of age, a BMI that is less than 70% of the average median BMI for that age
- in people under 18 years of age, refusing food completely or limiting consumption to less than 500 calories per day for more than 2 days
- recent weight loss (1 kg or more for 2 consecutive weeks)
- little or no nutrition for more than 5 days
- a pulse of less than 40 beats per minute
- a core body temperature less than 35°C
- sodium levels less than 130 mmol/l
- glucose or potassium levels less than 3 mmol/l
- elevated urea or creatinine
- abnormal heart rythms, for example bradychardia, particularly if the corrected QT interval is more than 450 ms.
The Sit Up, Squat–Stand (SUSS) Test is a physical assessment of muscle function. The patient is asked to sit up from lying on the floor, without using their hands, if possible, and then asked to stand from squatting, again without using their hands, if possible (see Figure 1).16 A SUSS score of 2 or less is also a red flag for anorexia.15 Liver function tests, phosphate, and creatine kinase levels also need to be measured.17,18
Patients with red-flag signs often need to be discussed with an acute medical team for possible inpatient management, and this may require a Mental Health Act assessment.17,18 However, if refeeding is commenced in the community, specialist nutritional advice is needed because of the risk of refeeding syndrome.17,18
Relapse rates are significant, and some patients have a relapsing–remitting course with a fluctuating weight over many years.2 An assessment of the patient’s bone mineral density may be needed, particularly in cases where there is amenorrhoea, or if underweight has persisted for more than 2 years (1 year in children and young people).5 In these circumstances, it is worth considering supplementation with vitamin D and calcium.19
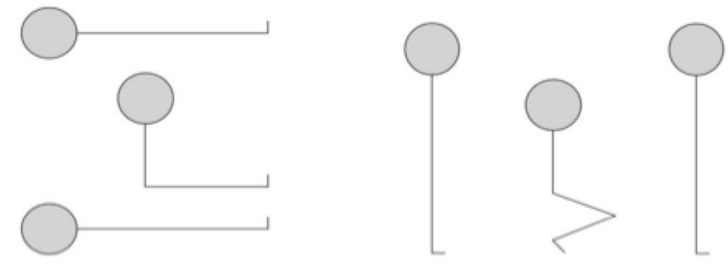
Robinson P. Avoiding deaths in hospital from anorexia nervosa: the MARSIPAN project. Psychiatrist 2012; 36 (3): 109–113. Reproducible under the creative commons CC-BY 4.0 licence.
Bulimia Nervosa
In patients with bulimia nervosa, as with anorexia, there is preoccupation with body image and/or weight, and impact on areas of daily life functioning.1 However, the individual’s weight is often not low, and it may even be high.11 Patients experience binges—periods where food intake is perceived to be outside of the person’s control, with an inability to stop or manage the type of food consumed.1 The episodes may only end when the person is so full that they are uncomfortable. In order to meet the criteria for the condition, these episodes occur at least weekly for a period of 1 month or more, and are accompanied by inappropriate compensatory mechanisms such as purging (for example, using laxatives or diuretics), self-induced vomiting, or excessive exercising.1 Binges are usually covert, and shame over the behaviour is common.11 In the author’s clinical experience, some people report that, rather than a sensation of loss of control, they experience a feeling of abandonment of effort to control their eating. If this is found on discussion with the patient, it should still be considered as one of the criteria for diagnosis.
As with anorexia, there may be a precipitating life event or prognostic factors—a history of anxiety, abuse, early puberty, overweight or obesity in childhood, or a history of depression, are pieces of the jigsaw that can alert healthcare professionals to the presence of the condition.2
Clinical Indications of Bulimia Nervosa
As with anorexia nervosa, other clinical findings may indicate the presence of bulimia. Self-induced vomiting can cause dyspepsia and oesophageal tears, as well as dental erosions, parotid swelling, and marking on the knuckles.11,12 Those using long-term laxatives may become dependent on them for bowel movements, or rectal prolapse may develop.2 Generalised abdominal symptoms may prompt consultation, so it is worth considering bulimia if nonspecific symptoms and signs are present with no obvious cause. Bulimia nervosa may also be an incidental finding due to electrolyte abnormalities, such as hypokalaemia, caused by purging behaviours.12 Arrhythmias may also occur as a consequence of hypokalaemia.12
Physical abnormalities are less common in patients with bulimia nervosa than in anorexia nervosa, but blood testing can be helpful. The picture may be one of hypokalaemia and/or hyponatraemia, raised bicarbonate levels, or elevated amylase (salivary isoenzyme) as a result of the purging methods used.2
Referral and Monitoring of Patients with Bulimia Nervosa
Although there is not typically the same level of physical ill health in patients with bulimia nervosa as there is in anorexia nervosa, individuals with this disorder have an elevated all-cause mortality rate,12 and prompt referral is associated with better outcomes.20 On the initial assessment, patients may not need such intensive physical monitoring as with anorexia.
In patients with either anorexia or bulimia, an explicit discussion should be had about possible drug and alcohol misuse, and suicidal ideation, as these are often associated with the illnesses.2 Interventions from the acute mental health team, drug and alcohol team, and eating disorders team may need to take place concurrently.
Binge Eating Disorder
Binge eating disorder is the most common eating disorder (after atypical eating disorders), and represents binge eating episodes of overeating with loss of control, and a sense of shame or guilt, along with a preoccupation with weight or shape.1 These binges typically occur at least weekly for 1 month or more but, unlike in bulimia, there are no regular compensatory behaviours.1 The quantity of food consumed is excessive—notably more than an average person would eat in the timeframe (typically up to 2 hours), and the person feels uncomfortably or painfully full.11 These episodes cause considerable distress.
Overweight or obesity are usually seen in patients with binge eating disorder,11 so taking a careful history when consulting about weight issues will help to assess patients with the disorder. Key features to look for are prominent depression or anxiety, a significantly high calorific intake, and functional impairment such as social withdrawal.11,12 Comorbid psychiatric conditions are also often found.21 Patients with binge eating disorder also require referral to eating disorder services, and although there is not usually an acute risk to physical health, assessment and management of weight-related conditions should be considered. Binge eating disorder should not be considered a lack of willpower or motivation; it is a recognised psychiatric condition and needs specialist assessment and management, with significant psychological intervention.5
Summary
Eating disorders are often under recognised, and in some cases individuals never present to services for help. Anorexia has a high mortality rate and requires physical assessment and monitoring, which can be quite intense. Bulimia and binge eating disorder are both characterised by periods of uncontrolled eating; the former with dysfunctional compensatory behaviours, which can result in physical ill health. All of these conditions require prompt referral to specialist eating disorder services, and general practice can signpost to sources of interim support, such as the charity Beat.14
Dr Emma Nash
GP and CCG lead for mental health, Hampshire

