Jackie Glatter and Dr Kevin Barrett Discuss the IBD UK Report on Services for People with Inflammatory Bowel Disease, Which Highlights Room for Improvement
| Read This Article to Learn More About: |
|---|
Find implementation actions for STPs and ICSs at the end of this article
  |
Delays to diagnosis, slow referral for specialist advice and treatment, and a lack of holistic, multidisciplinary care are the key findings of a new report into UK inflammatory bowel disease (IBD) services by IBD UK—an alliance of 17 professional bodies, medical royal colleges, and patient associations, including the Royal College of General Practitioners (RCGP), the Royal College of Nursing, and the Royal College of Physicians.1 The report—Crohn’s and colitis care in the UK: the hidden cost and a vision for change1—is based on the results of a unique assessment of care (Patient Survey and Service Self-Assessment) for IBD across the UK, involving over 70% of IBD services and more than 10,000 patients of all ages with IBD, and benchmarked against the 2019 consensus standards for the care of adults and children with IBD.1,2
The Burden of IBD
There are an estimated 500,000 adults and children with IBD in the UK, equating to one in every 133 people.1 IBD can be extremely debilitating, and has the potential to impact every aspect of the lives of people living with the condition. Symptoms of IBD can include urgent and frequent diarrhoea (often with blood and mucus), abdominal pain and fatigue, and the condition can also lead to anxiety and depression.1 Up to 50% of people living with IBD will experience extraintestinal manifestations, which affect the joints, skin, bones, eyes, kidneys, and liver.1,3 The impact of symptoms on the individual can be profound, leading to time off school or work, withdrawal from social relationships, and an inability to carry out everyday activities, such as shopping and exercise. Children living with IBD may experience delayed growth and development.4 The total lifetime cost of IBD is estimated to be equivalent to that for heart disease or cancer,5 given that most people are diagnosed with the condition between the ages of 15 and 40 years.1
Diagnosis of IBD
Delays to the diagnosis and treatment of IBD are associated with a reduced response to medical treatments and a higher incidence of urgent and emergency surgical interventions.6 People who are symptomatic and experience a delay prior to a diagnosis of Crohn’s disease or ulcerative colitis are more likely to undergo intestinal surgery.7
The Need for Improved Recognition of IBD
The findings of the IBD Patient Survey related to diagnosis are shown in Box 1.1
| Box 1: IBD Patient Survey Findings Related to Diagnosis1 |
|---|
IBD=inflammatory bowel disease |
The report highlights the challenges that need to be overcome to improve the diagnosis of IBD, including increasing awareness of Crohn’s disease and ulcerative colitis so that more people recognise the need to seek help from a healthcare professional.1 Symptoms may present atypically—for example, diarrhoea does not occur in all adults with IBD, and up to 44% of children with the condition do not experience diarrhoea.8 Other symptoms can include fever, weight loss, signs of malnutrition and malabsorption such as anaemia, inflammation of the joints, eyes, or skin, and mouth ulcers.9,10 Fifteen percent of individuals with IBD initially receive a diagnosis of irritable bowel syndrome (IBS),11 which indicates that IBD may not always be considered in line with optimal lower gastrointestinal symptom pathways. This includes people who were initially misdiagnosed with IBS, and those who develop IBD on a background of IBS—something that is currently poorly understood.
Best Practice in the Diagnosis of IBD
NICE Quality Standard 81 on IBD12 states that:
‘People with any of the following lower gastrointestinal symptoms that have been present for at least 6 weeks should be suspected of having inflammatory bowel disease:
- abdominal pain or discomfort
- bloating
- change in bowel habit (such as diarrhoea with or without rectal bleeding).’
IBD UK’s IBD standards state that clear pathways and protocols should be agreed between primary and secondary care for investigating children and adults with lower gastrointestinal symptoms, including guidance on the use of faecal biomarker tests in primary care to aid rapid diagnosis.13 In order to improve timely and appropriate referral and diagnosis, NICE recommends consistent and appropriate use of faecal calprotectin testing in primary care—as part of agreed referral pathways and protocols—in adults with recent lower gastrointestinal symptoms and for whom cancer is not suspected.14 Faecal calprotectin pathways have also been found to be beneficial for children with suspected IBD.15
A project led by the Yorkshire & Humber Academic Health Science Network has demonstrated that faecal calprotectin testing can reduce unnecessary appointments and colonoscopies, improve waiting times, and lead to financial savings (see Box 2).1
| Box 2: Best Practice—the York Faecal Calprotectin Pathway1 |
|---|
The Yorkshire & Humber Academic Health Science Network worked with York Teaching Hospital NHS Foundation Trust to develop a pathway for faecal calprotectin testing to improve diagnosis. This included providing templates and leaflets—for GPs and patients—to help them use and understand the process.
The pathway demonstrated a QALY benefit compared with all comparator pathways. By the end of 2019, the pathway had been rolled out to 71 CCGs in England. |
Managing Flares
Because IBD is a chronic, relapsing–remitting condition with potentially serious and life-threatening complications, timely management is essential. Progression of inflammation from untreated flares can lead to dehydration, malnutrition, bowel obstruction, fistulas, intestinal rupture or perforation, and an increased risk of cancer, and has an adverse impact on mental health.1
The Importance of Flare Pathways
The IBD Patient Survey findings related to managing flares are listed in Box 3.1
| Box 3: IBD Patient Survey Findings Related to Managing Flares1 |
|---|
IBD=inflammatory bowel disease |
A considerable number of patients reported contacting their GP in the first instance when they experienced a flare;1 therefore, it is important that GPs are able to respond appropriately and support patients to access specialist advice and treatment quickly, if needed. IBD UK’s IBD standards state that local treatment protocols and flare pathways should be in place for the management of patients with IBD experiencing flares, and that protocols should include advice for primary care (see Figure 1).16,17 The Inflammatory bowel disease toolkit, produced in partnership by the RCGP and Crohn’s & Colitis UK, includes flare pathways endorsed by the British Society of Gastroenterology and the Primary Care Society for Gastroenterology.18
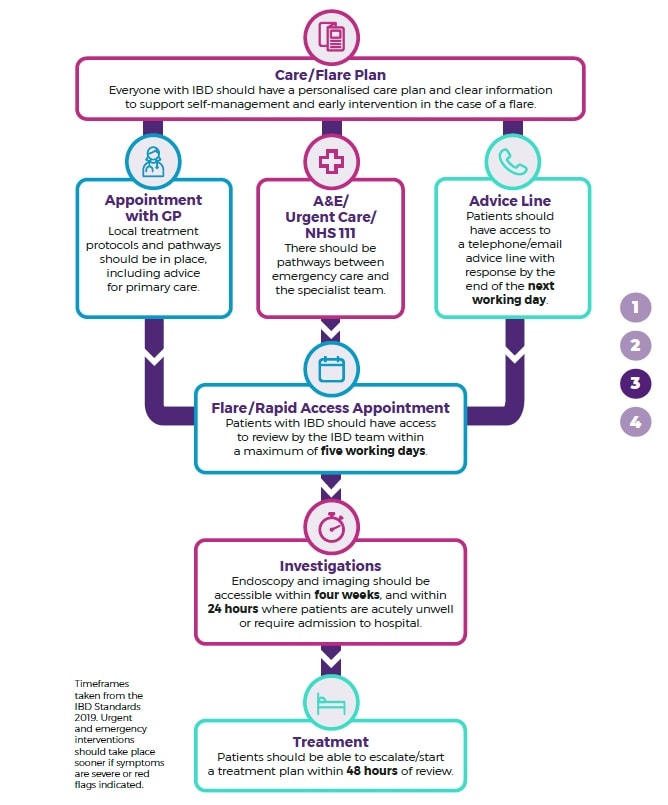
IBD=inflammatory bowel disease
Adapted from: IBD UK. Crohn’s and colitis care in the UK: the hidden cost and a vision for change. Hatfield: IBD UK, 2021. Available at: www.ibduk.org/reports/crohns-and-colitis-care-in-the-uk-the-hidden-cost-and-a-vision-for-change
Reproduced with permission
Coordinated Care
IBD is a complex condition, with emotional and physical effects that can vary hugely from one person to another. Good multidisciplinary team working is essential to deliver high-quality, coordinated, and personalised care.
The IBD Patient Survey demonstrated a range of positive outcomes associated with care that is well coordinated between gastroenterologists and GPs (see Box 4).1 However, the results also highlighted that fewer than half of those who responded to the survey felt that their care was well coordinated with other specialist services.1
| Box 4: IBD Patient Survey Findings Related to Coordinated Care1 |
|---|
IBD=inflammatory bowel disease |
Going Forward
The report concludes that coordination across primary and secondary care is of critical importance, and that GPs should be regarded as part of the broader care team for patients with IBD.1 It recommends that commissioners and managers should ensure that pathways are in place to deliver well-coordinated care across specialties, between adult and paediatric services, and between primary and secondary care (see Figure 2).1
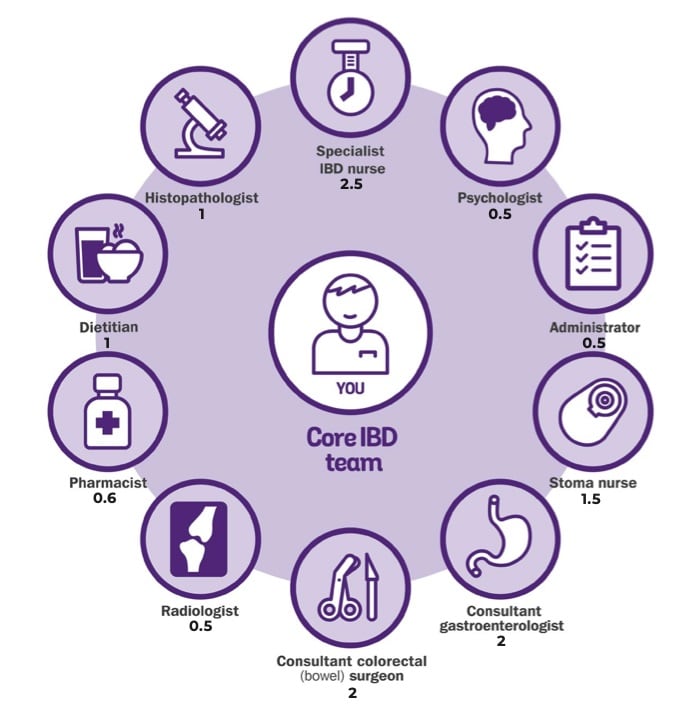
The IBD standards outline the range of professionals that should be included in the IBD team. For adult services, shown below each role is the number required per 250,000 catchment population.17
IBD=inflammatory bowel disease
Adapted from: IBD UK. Crohn’s and colitis care in the UK: the hidden cost and a vision for change. Hatfield: IBD UK, 2021. Available at: www.ibduk.org/reports/crohns-and-colitis-care-in-the-uk-the-hidden-cost-and-a-vision-for-change
Reproduced with permission
Summary
The IBD UK report reveals high levels of emergency treatment and a need for more personalised, proactive, and preventative care for patients with IBD, in line with the IBD standards. The coronavirus pandemic has exacerbated delays in investigation, diagnosis, and surgery. The report sets out some key goals for improved IBD care, including earlier diagnosis, more rapid access to specialists, and more personalised and joined-up multidisciplinary care. The IBD UK’s 17 professional and patient organisations are calling for greater prioritisation of IBD within the NHS, and a long-term strategy to improve care.
Jackie Glatter
Policy Manager, Crohn’s & Colitis UK
Dr Kevin Barrett
Chair, Primary Care Society for Gastroenterology
| Implementation Actions for STPs and ICSs |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved in implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
STP=sustainability and transformation partnership; ICS=integrated care system; IBD=inflammatory bowel disease |

