Dr Aisling MacCormac Provides Nine Top Tips on Managing the Symptoms of Sicca Syndrome in Primary Care
| Read This Article to Learn More About: |
|---|
|
1. Listen to the Patient’s Experience
Sicca syndrome can have a significant impact on the patient’s quality of life. Dry mouth can lead to problems with taste, chewing, swallowing, speaking, and halitosis, while dry eye causes ocular discomfort, blurring of vision and, in severe cases, damage and scarring to the cornea.1,2,4Few practitioners have the experience or equipment to perform objective measurements of salivary flow or tear film breakdown. It is therefore appropriate to classify the severity of symptoms according to the patient’s reports.
2. Consider and Address Underlying Causes Where Possible
Sicca syndrome may be idiopathic, iatrogenic, or occur secondary to Sjögren’s syndrome. Underlying causes are listed in Table 1, along with associated clinical features.
Table 1: Underlying Causes of Sicca Syndrome4–1
| Potential Underlying cause | Pathophysiology | Clinical Features | Diagnosis |
|---|---|---|---|
Drugs e.g.
| Antagonism of muscarinic receptors prevents parasympathetic activation of secretory cellsAntagonism of adrenergic receptors increases sympathetic stimulation and reduces output | May include other side-effects of medication | Careful drug history |
| Diabetes mellitus | Osmotic effects of hyperglycaemia causes dehydration | May be associated symptoms of hyperglycaemia e.g. polyuria, polydipsia, fatigue, recurrent skin infections | HbA1c or, where indicated, FPG |
| Reduced blinking e.g. prolonged screen use, Parkinson’s disease, deformity of the eyelid e.g. ectropion | Abnormal distribution of the tear film and increased evaporation from the surface of the eye | Associated features of neurological disorders | Examination of the external eye and neurological examination if indicated |
| Meibomian gland dysfunction/blepharitis | Reduced lipid content of tear film leads to increased evaporation from the surface of the eye | Inflammation of the eyelids and crusting at the base of the lashes. May be associated with rosacea or seborrhoeic dermatitis | Examination of the external eye |
| Laser eye or cataract surgery | Iatrogenic nerve damage leads to desensitivity and reduced glandular secretion | Gritty discomfort in the eyes Visual disturbances (e.g. glare) Red marks in the sclera | Ophthalmic history |
| Candidal infection | Infection by Candida albicans results in inflammation and sensation of xerostomia | White coating is seen on buccal mucosa, loss of papillae on tongue, and/or angular cheilitis is present | Identifying clinical features and ruling out differential diagnoses Swabs to detect C. albicans, or antibody serology, are generally not useful because candidal organisms are commonly found in healthy people |
| Anxiety | Increased sympathetic drive leads to reduction in salivary flow | Chronic, excessive worry unrelated to particular circumstances Restlessness, insomnia, muscle tension | A validated scoring tool e.g. GAD-7 may be used to assess severity of anxiety |
| Oral dysaesthesia or burning mouth syndrome | A neuropathic disorder causing oral dryness and discomfort without objective reduction in salivary flow | Dry mouth may be associated with a burning sensation or unusual taste Associated anxiety, depression | Clinical history to exclude underlying disease |
| Sjӧgren’s syndrome | Focal lymphocytic infiltration of exocrine glands May be a primary disorder or secondary to other autoimmune condition such as scLE or rheumatoid arthritis | Fatigue Arthralgia Associated autoimmune disease e.g. thyroid or coeliac disease, primary biliary cirrhosis | History of dry eye/mouth symptoms Positive anti-Ro and/or anti-La antibodies Objective ocular dryness (Schirmer’s test) Objective oral dryness (salivary scintigraphy, sialography) and labial biopsy may be considered in secondary care |
| Head and neck radiotherapy | Damage to salivary glands and oral mucosa when these are close to, or included in the field of radiation | In mucositis, erythema and ulceration of the oral cavity may be seen | Careful history taking |
| Sarcoidosis | Non-caseating granulomas form in salivary glands, reducing secretory function | Associated respiratory symptoms (non-productive cough, wheeze, shortness of breath), fatigue, myalgia | Classic chest X-ray findings, absence of autoantibodies, biopsy may be required |
| ACE=angiotensin converting enzyme; HbA1c =glycated haemoglobin; FPG=fasting plasma glucose; GAD-7=generalised anxiety disorder 7-item questionnaire; scLE=subacute cutaneous lupus erythematosus | |||
3. Consider Lifestyle Measures and Health Promotion
Oral health is of particular importance in those with xerostomia. Dietary sugars and acidic foods should be avoided as they encourage bacterial growth in patients already susceptible to dental decay. Teeth should be brushed twice a day with a soft toothbrush followed by rinsing with water or a fluoride or antiseptic mouthwash. Dentures should be removed at night and cleaned in accordance with dentists’ instructions.6Patients should be advised about maintaining adequate hydration. Sipping on water or sucking ice chips can help people who need to restrict fluid, such as those with congestive cardiac failure. A petroleum-based jelly can be helpful for cracked lips, while a water-based lubricant is appropriate for those on oxygen therapy.6
Smoking, caffeine, and alcohol are considered irritants and should be avoided or minimised. Reducing screen time and contact lens wearing may help symptoms of dry eye.1
4. Understand How Dry Eye Treatments Work
The tear film is made up of three layers covering the cornea and exposed conjunctiva: an inner mucin layer, a middle aqueous layer, and an outer lipid or meibomian layer, which prevents evaporation.1,20
Deficiency of the aqueous layer occurs because of reduced production in the lacrimal glands, for example, in Sjӧgren’s syndrome or because of excessive evaporation when the lipid layer is reduced.1 Measures designed to target aqueous deficiency may include humidification of the environment, wearing glasses to reduce evaporation, punctal plugging, and topical eye drops.1,4,20 Meibomian gland treatments may include lid hygiene and massage, or oral antibiotics such as doxycycline.21
5. Use a Stepwise Approach to Prescribing Eye Drops
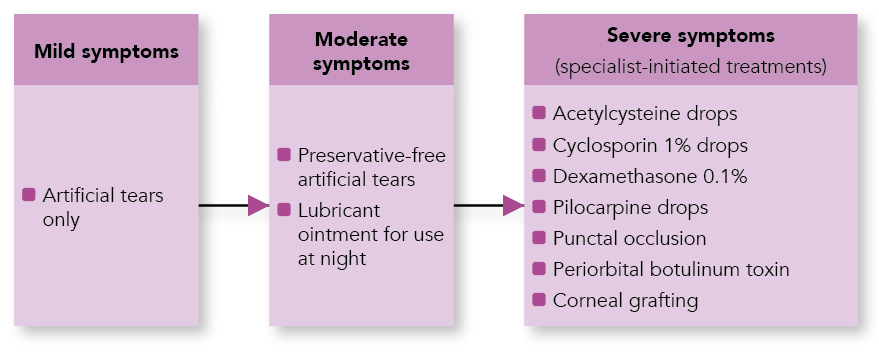
Artificial tears have been shown to slightly prolong the breakdown time of the tear film and reduce signs of ocular damage.1 Higher viscosity drops are designed to evaporate more slowly, providing longer term lubrication. However, there is not yet sufficient evidence to support the use of one product over another.1,20 Over-the-counter preparations may be as effective as those available only on prescription;20 therefore, clinicians should be guided by patient-reported symptoms and consider impact on quality of life.
Where symptoms persist despite topical treatments, it might be worth trialling a preservative-free treatment as irritation and allergy to preservatives can develop over time.1,5,20 Where this does not produce satisfactory symptom control, a higher viscosity product and/or a combination of treatments can be tried (see Figures 1 and 2).
Figure 1: Dry Eye Drops Classified According to their Viscosity4
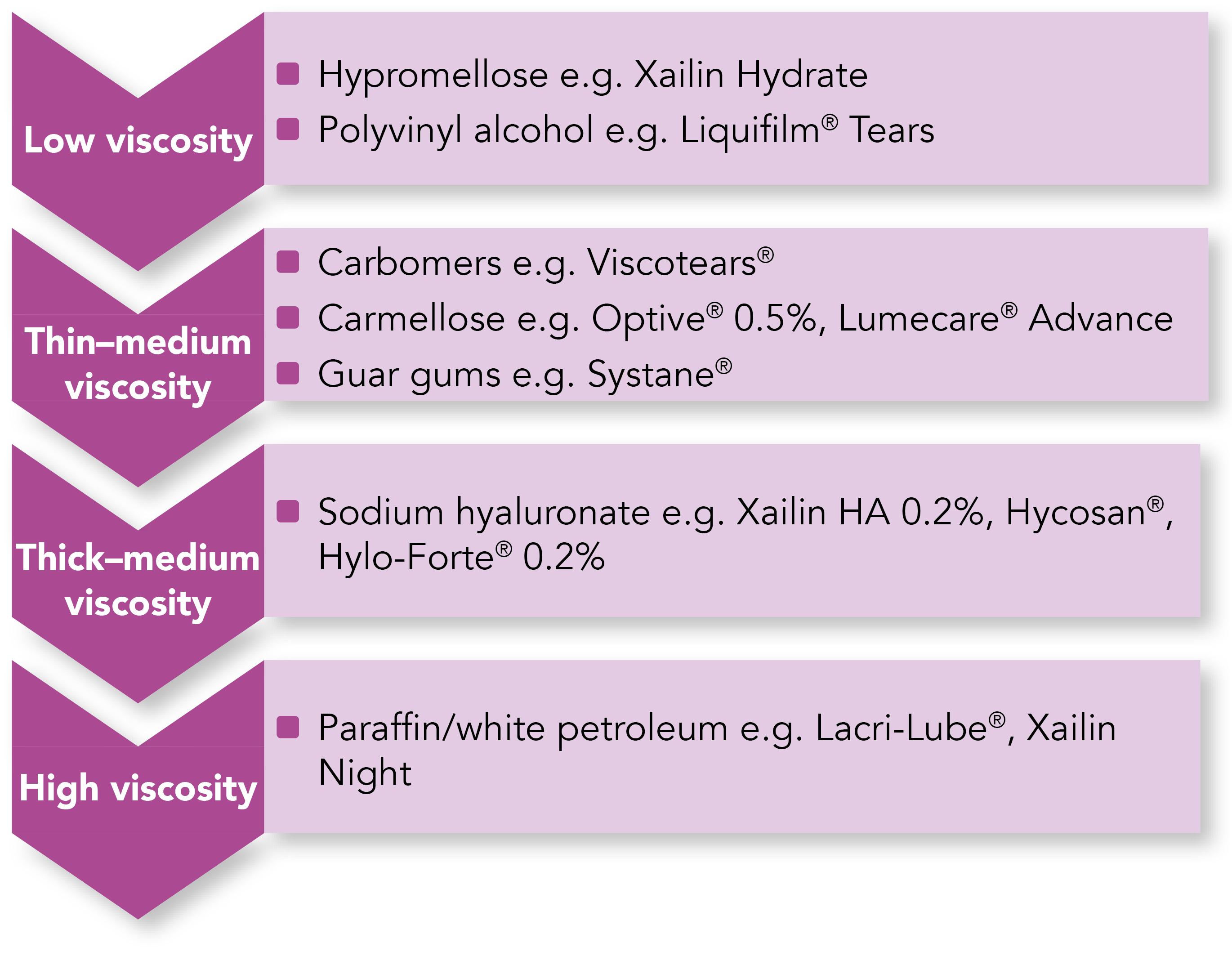
Figure 2: Escalating Treatment According to Symptom Severity4,5
6. Understand How Treatments for Dry Mouth Work
Saliva is produced continuously by the parotid, submandibular, and sublingual glands, with production increased by the sensory input of taste and smell, and the mechanical action of chewing.22
Salivary substitutes work by coating mucous membranes to reduce salivary loss by evaporation. Salivary stimulants work to increase production in those with residual salivary gland function, either pharmacologically or by mechanical action, such as chewing gum.2
Prescribing Dry Mouth Treatments
A 2011 Cochrane review2 evaluating topical treatments for xerostomia did not find strong evidence that topical treatments were superior to placebo, and there were few head-to-head trials comparing different products. Clinicians should, therefore, aim to try products with different active ingredients, as outlined in Table 2, until a patient preference can be established.
Table 2: Examples of Saliva Substitutes2
| Primary Lubricant | ||||
|---|---|---|---|---|
| Mucin | Glycerin | Carmellose | ||
| Antibacterial agent | Xylitol | AS Saliva Orthana® lozenges or spray | Oralieve spray and gel | |
| Xylitol, lactoperoxidase, lactoferrin, and others | Biotene Oralbalance® gel BioXtra® gel or spray | |||
| None | Saliveze® spray Xerotin® spray | |||
| Further information and more examples of saliva substitutes can be found at: bnf.nice.org.uk/medical-device-type/artificial-saliva-products-2.html | ||||
Pilocarpine is a muscarinic M3 receptor agonist which stimulates salivary flow.24 It is licensed for use in Sjӧgren’s syndrome and for xerostomia after radiotherapy.25 However, its use is contraindicated in poorly controlled asthma, chronic obstructive pulmonary disease, cardiorenal disease, and in those with uveitis. Side-effects include diarrhoea, nausea, hyperhidrosis, blood pressure instability, and disorders of vision, and it may take up to 3 months for the full effect of treatment to be seen.25
7. Review the Patient Regularly
To ensure maximum symptomatic benefit and to reduce waste, the efficacy of prescribed treatments should be reviewed after 4–6 weeks, and if symptoms remain inadequately controlled, consideration should be given to switching products.5
8. Screen for Other Manifestations of Sicca Syndrome Impacting on Quality of Life
The symptoms of sicca syndrome may extend beyond dry eyes and mouth to include chronic cough and vaginal dryness in women.4 These symptoms should be screened for as part of routine review and appropriate symptomatic treatments offered.
9. Know When to Refer
Same-day ophthalmology referral should be considered where there is moderate/severe eye pain or photophobia, unilateral red eye, or reduced visual acuity.1 Indications for non-urgent referral to ophthalmology include:4,5
- underlying pathology requiring specialist input, such as Sjӧgren’s syndrome
- treatment failure
- diagnostic uncertainty
- deteriorating vision
- evidence of corneal damage.
Urgent medical referral is required for dry mouth where there is significantly reduced oral intake, mucositis causing severe pain, suspected neutropenic mouth ulcers, or severe/persistent candida or herpes simplex virus infection.6 Referral to a dietitian and/or speech and language therapy service may be appropriate when there is reduced nutritional intake, dysphagia, or speech impairment.6
Summary
Sicca syndrome is a common condition with a range of aetiologies including prescribed medications, diabetes, ophthalmological disorders, and Sjögren’s syndrome. First-line management strategies include lifestyle modification and addressing underlying causes where possible. A wide range of artificial saliva and tear replacement products are available but in the absence of evidence directly comparing them, it is appropriate to trial a range of products and prescribe in accordance with patient preference. Clinicians should seek specialist review where there is treatment failure, diagnostic uncertainty, or evidence of complications such as deteriorating vision.
Dr Aisling MacCormac
GPwSI palliative care, North Yorkshire

