Professor Peter J Grant and Professor Francesco Cosentino Highlight the Key Recommendations from the 2019 ESC/EASD Guideline on Diabetes, Pre-diabetes, and CVD
| Read This Article to Learn More About: |
|---|
Find key points and implementation actions for STPs and ICSs at the end of this article |
The prevalence of diabetes continues to rise; an estimated 60 million people in Europe were thought to have the condition in 2017 and predictions suggest it will affect more than 600 million worldwide by 2045.1 These numbers carry a huge burden of morbidity and mortality with a high prevalence of microvascular disease affecting the eyes, nerves, and kidneys, and macrovascular disease leading to cardiovascular disease (CVD), cerebrovascular disease, and lower extremity artery disease (LEAD).
The combination of diabetes, chronic kidney disease (CKD), hypertension, and dyslipidaemia contribute to the development of CVD. The 2019 guideline on diabetes, pre-diabetes, and cardiovascular diseases from the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD)1 pays particular attention to the new information from clinical trials that address the management of these issues. While the recommendations have been updated, the emphasis remains on the importance of making individualised care decisions in collaboration with other healthcare professionals and informed patients as outlined in the 2013 guideline.2
This article focuses on the updated recommendations in the 2019 ESC/EASD guideline on diabetes, pre-diabetes, and cardiovascular diseases that are relevant to primary care.
Major Recommendations
Diagnosis of Diabetes
In many cases, a diagnosis of diabetes in primary care is clear, in part because many patients are symptomatic, but also because their fasting plasma glucose (FPG) is markedly elevated. In patients who present with underlying CVD or who are being investigated for other reasons (e.g. strong family history), it is now recognised that the first diagnostic approach should be to measure the HbA1C (>6.5%, 48 mmol/mol) and FPG (>7.0 mmol/l, 126 mg/dl).1 If the results are equivocal, tests can initially be repeated followed by an oral glucose tolerance test if a high level of suspicion persists.
Classification of Cardiovascular Risk in Diabetes
In recognition of the complexity of CVD in diabetes and to harmonise with other ESC guidelines we have adopted a recommendation with three levels of risk: very high, high, and moderate (see Table 1).1
This approach supersedes the use of the terms primary and secondary prevention which provide less accurate definitions of CVD. Acknowledging the importance of individualised care, it is anticipated that these changes will support appropriate diagnostic and therapeutic approaches to patient care.
Table 1: Cardiovascular Risk Categories in People with Diabetes1
| Risk Category | Risk Factors |
|---|---|
| Very high risk | Patients with DM and established CVD
|
| High risk | Patients with DM duration ≥10 years without target organ damage plus any other additional risk factor |
| Moderate risk | Young patients (T1DM aged <35 years or T2DM aged <50 years) with DM duration <10 years, without other risk factors |
a Proteinuria, renal impairment defined as eGFR ≥30 ml/min/1.73 m2, left ventricular hypertrophy, or retinopathy b Age, hypertension, dyslipidaemia, smoking, obesity | |
| DM=diabetes mellitus; CVD=cardiovascular disease; T1DM=type 1 diabetes mellitus; T2DM=type 2 diabetes mellitus; eGFR=estimated glomerular filtration rate | |
| Francesco Cosentino, Peter J Grant, Victor Aboyans et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). European Heart Journal 2019 00: 1–69. doi:10.1093/eurheartj/ehz486. Reprinted by permission of Oxford University Press on behalf of the European Society of Cardiology. Please visit: www.escardio.org/Guidelines | |
Blood Pressure Targets
Recommendations for blood pressure (BP) targets have been modified to consider the effects of age and co-morbidities. A systolic BP of >120 mmHg and <130 mmHg is recommended in younger patients with diabetes, and a systolic BP of >130 mmHg and <140 mmHg in patients aged over 65 years.1 The diastolic BP target is <80 mmHg, but not <70 mmHg.1 These targets may be modified according to the presence of other disorders and the patient’s ability to tolerate treatment.
Lipid Targets
The development of proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors has made it possible to achieve low levels of low-density lipoprotein cholesterol (LDL-C), which were previously not achievable with statins and ezetimibe. In line with this development, the recommendations for LDL-C targets are based on the patient’s risk of CVD:1
- LDL-C of <2.5 mmol/l (100 mg/dl) for people with diabetes at moderate risk of CVD
- LDL-C of <1.8 mmol/l (<70 mg/dl) for people with diabetes at high risk of CVD
- LDL-C of <1.4 mmol/l (55 mg/dl) for people with diabetes at very high risk of CVD.
Patients at moderate and high risk of CVD can usually be managed using maximal statins, with or without ezetimibe. However, in patients at very high risk of CVD, with persistently elevated LDL-C levels despite maximal statin therapy, a PCSK9 inhibitor is recommended.1
Aspirin Therapy
Aspirin therapy is established in the secondary prevention of CVD, but the precise positioning of aspirin across the spectrum of diabetes has been more controversial. The recent A Study of Cardiovascular Events iN Diabetes (ASCEND) trial revisited this issue in a randomised controlled trial (RCT) of more than 15,000 patients who had diabetes but no CVD, randomised to receive aspirin 100 mg daily or placebo.3 Aspirin was associated with a relative risk reduction of 12% and a relative risk of major bleeding of 1.29. These results are in line with other studies (as discussed in the guideline1) of moderate to high risk, formerly primary prevention, and the ESC/EASD guideline therefore recommends that aspirin may be considered on an individual basis in the absence of contraindications in patients with diabetes who are at high or very high risk of CVD. In patients with diabetes who are at moderate risk of CVD, aspirin is not recommended.1
Novel Oral Anticoagulants
Non-vitamin K antagonist oral anticoagulants (NOACs), such as dabigatran, rivaroxaban, apixaban, and edoxaban, directly inhibit the activated factor X complex in the coagulation cascade, thereby reducing thrombin generation, clot formation, and platelet activation.
NOACs have taken the place of warfarin in the management of patients with atrial fibrillation, deep vein thrombosis, and pulmonary embolus. However, recent data from the Cardiovascular Outcomes for People Using Anticoagulation Strategies (COMPASS) trial of rivaroxaban in patients with stable atherosclerotic disease—38% of whom had diabetes—indicated that rivaroxaban plus aspirin caused a significant reduction in the primary end point of myocardial infarction, stroke, or cardiovascular (CV) death compared with aspirin alone. Of perhaps greater significance in diabetes, in patients with LEAD there was a 46% reduction in major amputations.4
These findings led to recommendations that NOACs should be used in people with diabetes with atrial fibrillation, and that low-dose rivaroxaban in combination with aspirin should be considered in high-risk patients with diabetes and in patients with LEAD.1
Dual Antiplatelet Therapy
Dual antiplatelet therapy is now recommended for up to 3 years, in place of the previous recommendation of 12 months, in patients with diabetes post-acute coronary syndromes who have no evidence of life-threatening bleeding.1
Cardiovascular Safety Trials
The last 10 years have seen a plethora of CV safety trials, initiated by the US Food and Drug Administration, in response to a meta-analysis that indicated that the glucose-lowering drug rosiglitazone increased CV risk.5
Three new families of therapies have been tested in large-scale randomised control trials (RCTs) to assess CV safety and benefit. These are dipeptidyl peptidase-4 (DPP-4) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists, which act on the incretin system, and sodium-glucose co-transporter-2 (SGLT-2) inhibitors, which act on the proximal tubule of the kidney to block urinary glucose re-uptake.
DPP-4 inhibitors showed no increased risk of non-fatal myocardial infarction or stroke or of CV death, but no CV benefit; however, saxagliptin displayed an increased risk of hospitalisation for heart failure.1
In contrast, in the Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results (LEADER) trial6 and the Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes (SUSTAIN-6),7 the GLP-1 receptor agonists liraglutide and semaglutide showed both CV safety and CV benefit.
Likewise, the EMPA-REG OUTCOME trial,8 the Canagliflozin Cardiovascular Assessment Study (CANVAS),9 and the Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE–TIMI 58) trial10 found the SGLT-2 inhibitors empagliflozin, canagliflozin, and dapagliflozin to have both CV safety and CV benefit.
These results led the ESC/EASD guideline to recommend an SGLT-2 inhibitor or a GLP-1 receptor agonist as first-line treatment to reduce CV events in newly diagnosed, drug-naïve patients with type 2 diabetes at high or very high CV risk, and first-line empagliflozin or liraglutide to reduce the risk of death in patients at high or very high CV risk.1
All the reported SGLT-2 inhibitor trials showed significant reductions in hospitalisation for heart failure and are recommended in heart failure if the estimated glomerular filtration rate (eGFR) is stable and >30 ml/min/1.73m2.1
All the SGLT-2 inhibitors also showed renal benefit as a secondary end point and canagliflozin has now been tested in a renal primary end point trial, Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE), which was stopped early after an interim analysis reported superiority.11 SGLT-2 inhibitors should be considered if the eGFR is 30–90 ml/min/1.73 m2.1 GLP-1 receptor agonists semaglutide and liraglutide were also associated with a lower risk of renal end points and should be considered if the eGFR is >30 ml/min/1.73m2.1
Metformin
Metformin was previously recommended as first-line treatment in all overweight patients with type 2 diabetes following the results of a nested study extracted from the UK Prospective Diabetes Study (UKPDS).12
In light of the findings from the recent CV outcome trials, the ESC/EASD guideline now recommends that metformin can be considered as first-line therapy in overweight, drug-naïve, newly diagnosed patients with type 2 diabetes without CVD or high/very high CV risk. SGLT-2 inhibitors or GLP-1 receptor agonists should be first-line treatment in overweight, drug-naïve, newly diagnosed patients with type 2 diabetes with CVD or high/very high CV risk (Figure 1).1 Figure 2 outlines the management of patients with type 2 diabetes who are already on metformin.
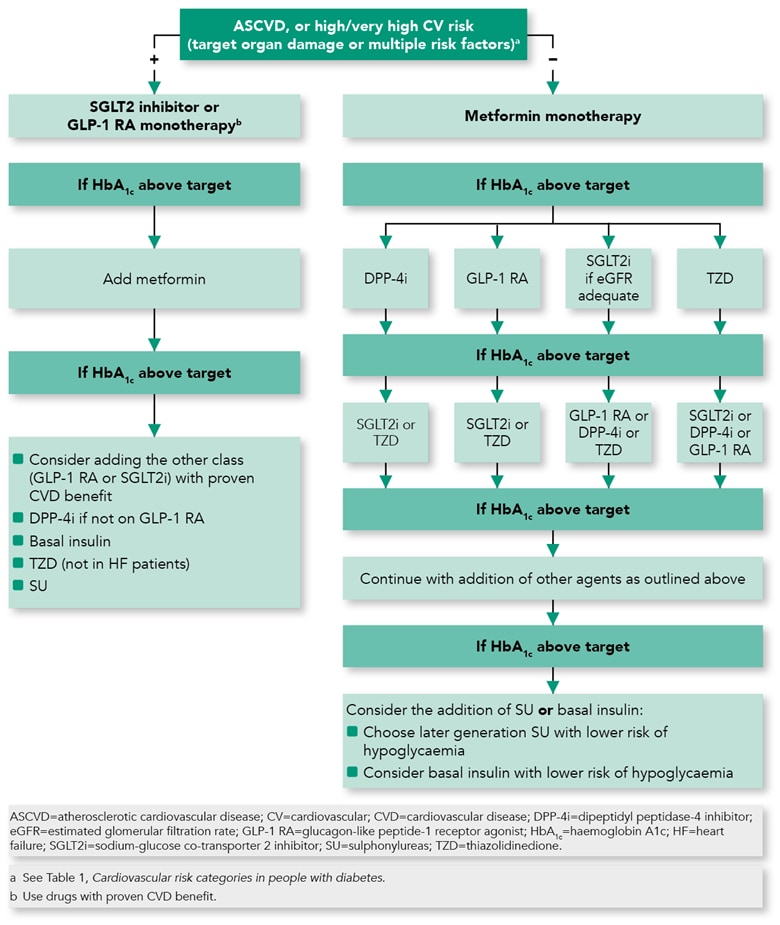
Francesco Cosentino, Peter J Grant, Victor Aboyans et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). European Heart Journal 2019; 00: 1–69. doi:10.1093/eurheartj/ehz486. Reprinted and modified by permission of Oxford University Press on behalf of the European Society of Cardiology. Please visit: www.escardio.org/Guidelines
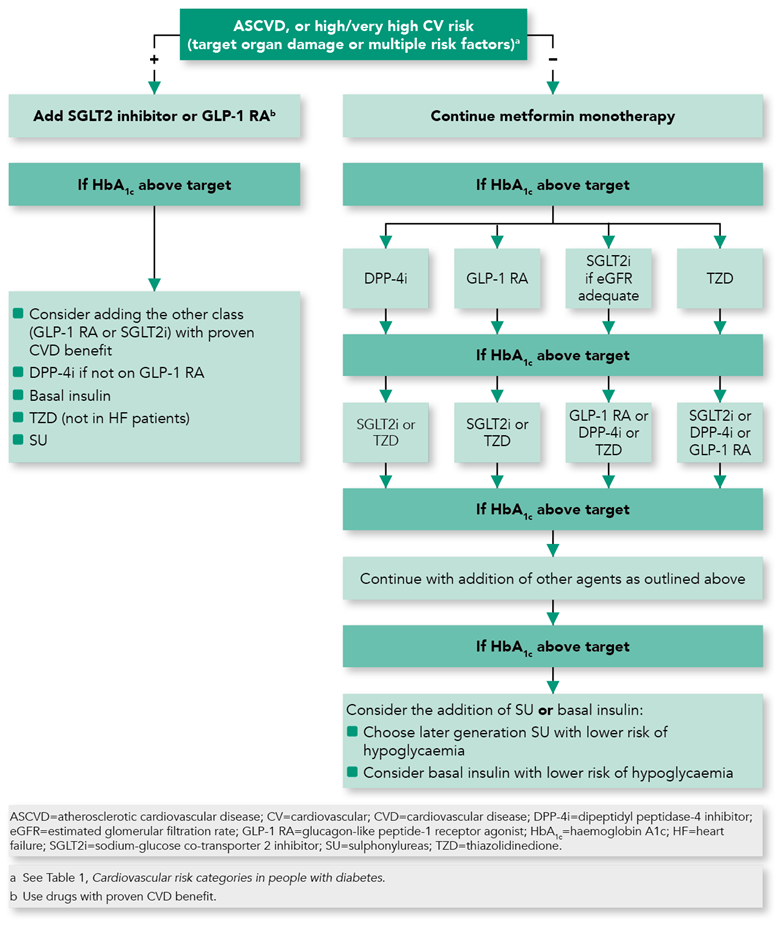
Francesco Cosentino, Peter J Grant, Victor Aboyans et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). European Heart Journal 2019; 00: 1–69. doi:10.1093/eurheartj/ehz486. Reprinted and modified by permission of Oxford University Press on behalf of the European Society of Cardiology. Please visit: www.escardio.org/Guidelines
Coronary Artery Revascularisation
In general, with more complex disease presentation it is recommended to revascularise patients with diabetes by coronary artery bypass graft (CABG) rather than percutaneous coronary intervention (PCI) if they have stable coronary artery disease (CAD) and suitable anatomy for both procedures. The evidence for the use of CABG in three-vessel CAD and left main CAD is stronger than for the use of PCI except in low complexity left main disease where both CABG and PCI are recommended as equally valid options.1 The same revascularisation techniques, that is, the use of drug-eluting stents and the radial approach for PCI and the use of the left internal mammary artery as the graft for CABG, are recommended in patients with and without diabetes.1
Summary
Diabetes is associated with a two- to three-fold increase in CVD, a figure which increases markedly in patients with young-onset, long-duration diabetes and in the presence of co-morbidities (previous vascular events, CKD, and risk factor clustering).
Clinical studies indicate that simple improvements in glycaemic control reduce the risk of developing microvascular disease (eyes, nerves, and kidneys) but have little beneficial effect on CVD in the medium term.1 The importance of co-morbidities and risk clustering have stimulated the need to manage CV risk factors aggressively to prevent the development of CVD. To aid in this process, a new CV risk stratification is presented to simplify management decisions and to acknowledge the complexity of disease management in diabetes. Unfortunately, there remains strong evidence that despite major advances in our understanding of how to ameliorate CVD in patients with diabetes, most are undermanaged and do not achieve treatment goals.13
All healthcare professionals who manage patients with diabetes should provide them with clear education and appropriate care consonant with each individual’s risk profile. In general, the younger a patient is at diagnosis, the more life years will be lost with poor diabetes management. In this group, aggressive treatment to improve glycaemic control and to achieve other risk targets (BP, lipids, and antiplatelet agents) is important.
In addition, whatever treatment modalities are used (drug therapies, PCI with stents, or CABG), patients with diabetes generally have worse outcomes than those without the disease, a difference referred to as residual risk. The cause of residual risk remains unclear; until the cause is identified it further emphasises the need to treat CV risk factors to target in all patient groups. Bearing in mind the importance of early management, in all individuals who present with vascular events, FPG and HbA1c should be measured to exclude the presence of diabetes and to support appropriate individualised care.
The new guideline has been produced to aid the appropriate management of dyslipidaemia and BP, in both instances by using the new CV risk classification.
Finally, perhaps the major novel recommendations in the management of patients with type 2 diabetes involve the repositioning of metformin, SGLT-2 inhibitors, and GLP-1 receptor agonists. The guideline recommends that metformin should remain first-line therapy in overweight, drug-naïve, newly diagnosed patients with type 2 diabetes without CVD or who are not at high or very high CV risk,1 which the committee thought was in line with the original UKPDS results.12 However, in overweight, drug-naïve, newly diagnosed patients with type 2 diabetes with CVD or who are at high or very high CV risk, either an SGLT-2 inhibitor or a GLP-1 receptor agonist should be used as first-line treatment. The latter recommendations are consistent with the reductions in CV outcomes and amelioration of the renal impairment deterioration reported consistently with both groups of agents.
Professor Peter J Grant
Guideline Chair representing the European Association for the Study of Diabetes; Professor of Medicine, University of Leeds
Professor Francesco Cosentino
Guideline Chair representing the European Society of Cardiology; Professor of Cardiology, Karolinska University Hospital, Stockholm, Sweden
Acknowledgements
Producing these guidelines has been a labour of love over the last 2 years and could not have taken place without the support provided by the members of the Guidelines Task Force and the ESC Guidelines Team led by Veronica Dean.
| Key Points |
|---|
ESC=European Society of Cardiology; EASD=European Association for the Study of Diabetes; HbA1c =haemoglobin A1c; FPG=fasting plasma glucose; CV=cardiovascular; BP=blood pressure; NOACs=non-vitamin K antagonist oral anticoagulants; AF=atrial fibrillation; ACS=acute coronary syndromes; CVOTs=cardiovascular outcome trials; SGLT-2=sodium-glucose co-transporter-2; GLP-1 RA=glucagon-like peptide-1 receptor agonist; CVD=cardiovascular disease; CKD=chronic kidney disease; CABG=coronary artery bypass graft; PCI=percutaneous coronary intervention; CAD=coronary artery disease |
| Implementation Actions for STPs and ICSs |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon The following implementation actions are designed to support STPs and ICSs with the challenges involved with implementing new guidance at a system level. Our aim is to help you consider how to deliver improvements to healthcare within the available resources.
STP=sustainability and transformation partnership; ICS=integrated care system |

