Muhammad Siddiqur Rahman Explores How Pharmacists Can Help Adults with Hypertension Meet Their Blood Pressure Targets and Optimise Their Medication
| Read This Article to Learn More About: |
|---|
|
Hypertension is defined by the World Health Organisation (WHO) as persistently raised high blood pressure (BP),1 and affects more than 1 in 4 adults in the UK.2 Hypertension increases the risk of cardiovascular and related diseases, including heart attacks, strokes, heart failure, and chronic kidney disease (CKD).2 Globally, around one-half of all deaths from stroke and heart disease are attributable to hypertension.1
NHS health checks, ‘well man’ or ‘well woman’ clinics run by healthcare assistants (HCAs) or nurses, and medical examinations by GPs all provide useful opportunities for identifying people who are at risk of hypertension. Patients who are at risk of hypertension may also be identified incidentally by practice-based pharmacists during medication reviews or clinics for related chronic conditions. Such opportunities can help ensure that people with hypertension are diagnosed promptly by the GP, recorded on the hypertension register, and started on treatment. Practice-based pharmacists can then be involved with managing patients with hypertension by conducting ongoing patient reviews and optimising antihypertensive medication, while also providing non-pharmacological intervention advice.
Note: NICE is expected to publish an updated guideline on the diagnosis and management of hypertension in adults in August 2019. This article makes reference to recommendations detailed in the draft version3 of the guideline, which may differ from those included in the final publication. Readers are advised to refer to the final version of the 2019 NICE hypertension guideline on publication.
Diagnosing Hypertension
If a clinic BP reading is between 140/90 mmHg and 180/110 mmHg then the patient is considered at risk of hypertension. The NICE guideline recommends that ambulatory blood pressure monitoring (ABPM) is used to confirm the diagnosis. Refer patients with a BP of 180/110 mmHg or higher to the GP to investigate possible severe hypertension. See Box 1 for the NICE clinical definitions for different levels of severity (‘stages’) of hypertension.
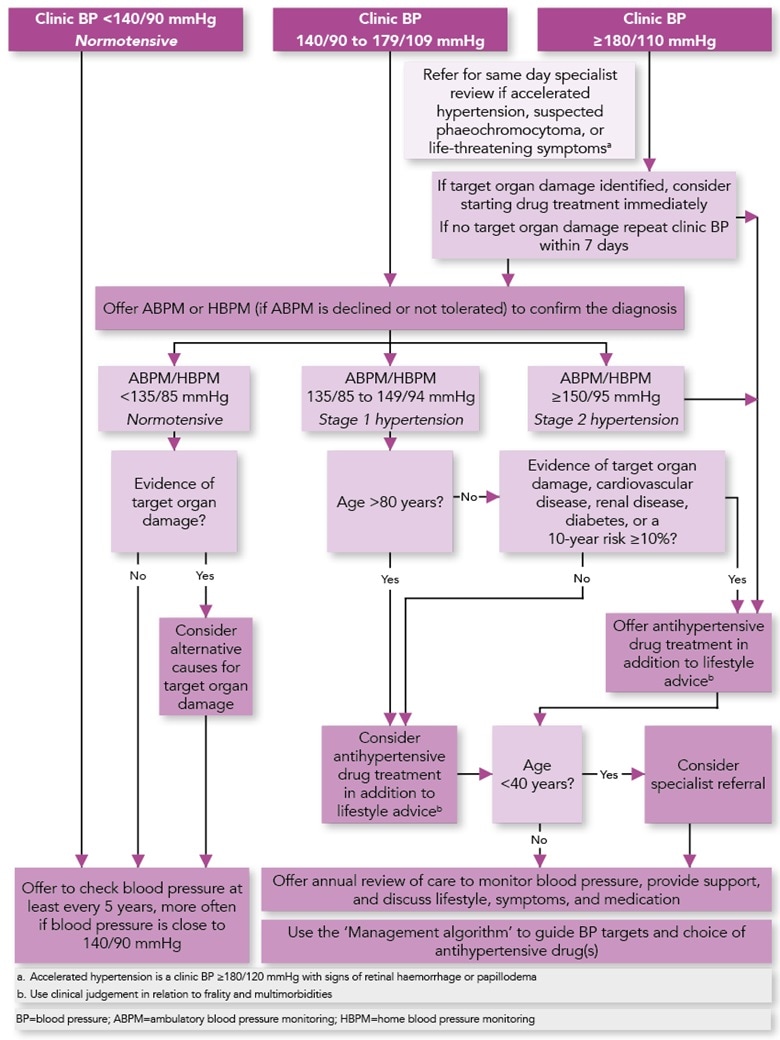
The algorithm in Figure 1 summarises the diagnosis and treatment initiation pathway for patients with hypertension (excluding diabetes or pregnancy).
| Box 1: NICE Clinical Definitions of Hypertension3 |
|---|
Stage 1 hypertension: clinic BP ranging from 140/90 mmHg to 159/99 mmHg and subsequent ABPM daytime average or HBPM average BP ranging from 135/85 mmHg to 149/94 mmHg. Stage 2 hypertension: clinic BP of 160/100 mmHg or higher but less than 180/110 mmHg and subsequent ABPM daytime average or HBPM average BP of 150/95 mmHg or higher. Stage 3 or severe hypertension: clinic systolic BP of 180 mmHg or higher or clinic diastolic BP of 110 mmHg or higher. BP=blood pressure; ABPM=ambulatory blood pressure monitoring; HBPM=home blood pressure monitoring © NICE 2019. Hypertension in adults: diagnosis and management—draft for consultation, March 2019. Available from: www.nice.org.uk/guidance/indevelopment/gid-ng10054/documents All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication |
© NICE 2019. Hypertension in adults: diagnosis and management—draft for consultation, March 2019. Available from: www.nice.org.uk/guidance/indevelopment/gid-ng10054/documents All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication
Taking Blood Pressure Measurements
When using an automated BP monitor, the patient should be seated for 5 minutes with the arm supported at heart level.4 Devices for measuring BP must be properly validated, maintained, and regularly recalibrated according to the manufacturer’s instructions.3,4
Automated devices may not produce an accurate measurement if the patient has an irregular pulse. NICE recommends palpating the radial or brachial pulse before measuring BP to check for pulse irregularity, and if there is any irregularity, measure BP manually using direct auscultation over the brachial artery.3 Any pulse irregularity could be a sign of another condition, such as atrial fibrillation, so the patient should be referred to the GP for further investigation.5
Some patients may exhibit a ‘white-coat effect’ (clinic BP exceeds average daytime ABPM BP or average HBPM BP measurements by more than 20/10 mmHg), or masked hypertension (clinic BP measurements are normal [less than 140/90 mmHg], but are higher when taken using ABPM or HBPM outside the clinic). In these cases, consider adjunctive ABPM or HBPM alongside clinic BP readings to monitor response to treatment or lifestyle modification.3
Further Investigations
Investigations should also be carried out to determine if there is evidence of target organ damage, such as left ventricular hypertrophy or chronic kidney disease (CKD):3
- test for proteinuria by sending a urine sample for estimation of albumin:creatinine ratio and test for haematuria
- measure glycated haemoglobin (HbA1c), electrolytes, creatinine, estimated glomerular filtration rate (eGFR), serum total cholesterol, and high-density lipoprotein cholesterol
- examine fundi for presence of hypertensive retinopathy
- arrange a 12-lead electrocardiogram (ECG).
The GP should also conduct a formal assessment of cardiovascular risk using a cardiovascular risk assessment tool. Where the patient has signs or symptoms suggestive of an underlying cause (i.e. secondary hypertension), consider whether there is a need for specialist investigations.3
Routine Blood Pressure Monitoring
Adults with hypertension should be reviewed at least once a year to monitor BP, provide support, and discuss lifestyle, symptoms, and medication.3
If hypertension is not diagnosed after ABPM or HBPM, the patient should be invited back for routine BP monitoring at least once every 5 years, and more frequent measurements should be considered if their clinic BP is close to 140/90 mmHg.3
Treatment Targets
Blood pressure targets should be agreed within the practice in line with the quality and outcomes framework (QOF) part of the General Medical Services (GMS) contract.6 Therapeutic targets according to the QOF and the NICE guideline are shown in Table 1.3,6
Table 1: Therapeutic Targets for Hypertension
| BP Measured in Clinic | ABPM Daytime Average or HBPM Average | |||
|---|---|---|---|---|
| No diabetes | Diabetes | No diabetes | Diabetes | |
| QOF standard6 | ≤140/90 mmHg (if aged <80 years) measured in the preceding 12 months ≤150/90 mmHg (if aged ≥80 years) measured in the preceding 12 months | ≤140/80 mmHg measured in the preceding 12 months, without moderate or severe frailty | The contractor may be required by commissioners to discuss their plans for ensuring that new diagnoses [of hypertension] are confirmed using ABPM or HBPM as appropriate. | |
| NICE guidance3 | <140/90 mmHg in adults aged <80 years <150/90 mmHg in adults aged ≥80 years (use clinical judgement for people with frailty or multimorbidity) | Type 2 diabetes: targets are the same as in those without type 2 diabetes | <135/85 mmHg for adults aged <80 years <145/85 mmHg for adults aged ≥80 years | Type 2 diabetes: targets are the same as in those without type 2 diabetes |
Type 1 diabetes:7<135/85 mmHg <130/80 mmHg if albuminuria or 2 or more features of metabolic syndrome | Type 1 diabetes:7 ABPM/HBPM targets not specified | |||
In people with symptoms of postural hypotension (falls or postural dizziness):
Measure standing BP in adults with hypertension who have type 2 diabetes, symptoms of postural hypertension, or are aged 80 years or over Treat to a target based on standing BP in people with a significant postural drop or symptoms of postural hypotension. | ||||
| The QOF also includes BP indicators for other related conditions. Please see the full version of the QOF for BP related standards for the secondary prevention of coronary heart disease, stroke and transient ischaemic attack, and mental health. | ||||
| BP=blood pressure; ABPM=ambulatory blood pressure monitoring; HBPM=home blood pressure monitoring; QOF=Quality and Outcomes Framework | ||||
Non-pharmacological Interventions
Lifestyle intervention is an important element of hypertension management. Advice on lifestyle can be offered by HCAs and practice nurses initially, then followed up by GPs and pharmacists. Lifestyle modifications can help reduce BP and hence the need for medication, as well as reducing the risk of developing cardiovascular disease (CVD).8
NICE recommends the following non-pharmacological interventions to manage and prevent high BP in adults:3
- ascertain a patient’s diet and offer appropriate written or audiovisual advice:
- pharmacist prescribers can also consider prescribing orlistat for weight loss as part of an overall plan for managing obesity, in line with NICE Clinical Guideline 189, Obesity: identification, assessment and management9
- recommend regular physical exercise
- advise reduced consumption of sodium salt
- encourage reduced intake of alcohol if they drink excessively
- discourage excessive caffeine consumption
- offer advice and help smokers to stop smoking
- signpost to local initiatives to provide support and promote healthy lifestyle change.
See Box 2 for some resources to help guide lifestyle interventions.
| Box 2: Resources for Guiding Lifestyle Interventions |
|---|
These resources are applicable to the general population but will be of particular help in reducing cardiovascular disease risks associated with hypertension, or in reducing blood pressure. NHS.uk Advice and GuidelinesNICE GuidelinesClinical Guideline 43: Obesity prevention Clinical Guideline 189: Obesity: identification, assessment and management Public Health Guideline 25: Cardiovascular disease prevention Clinical Guideline 181: Cardiovascular disease: risk assessment and reduction, including lipid modification NICE Guideline 92: Stop smoking interventions and services |
The Dietary Approaches to Stop Hypertension (DASH) diet is currently gaining momentum in the USA and has been shown to reduce average BP by around 8–14 mmHg. The DASH diet is rich in fruits, vegetables, and low-fat dairy, with reduced saturated fat, total fat, and sodium intake.10,11
Pharmacological Interventions
Commencement of antihypertensive medication is usually carried out by the GP, based on the stage/severity of hypertension as per NICE guidelines (see Box 1) as well as any other co-morbidities or risks. For more information on appropriate choice of pharmacological interventions, refer to the NICE stepwise algorithm (Figure 2).
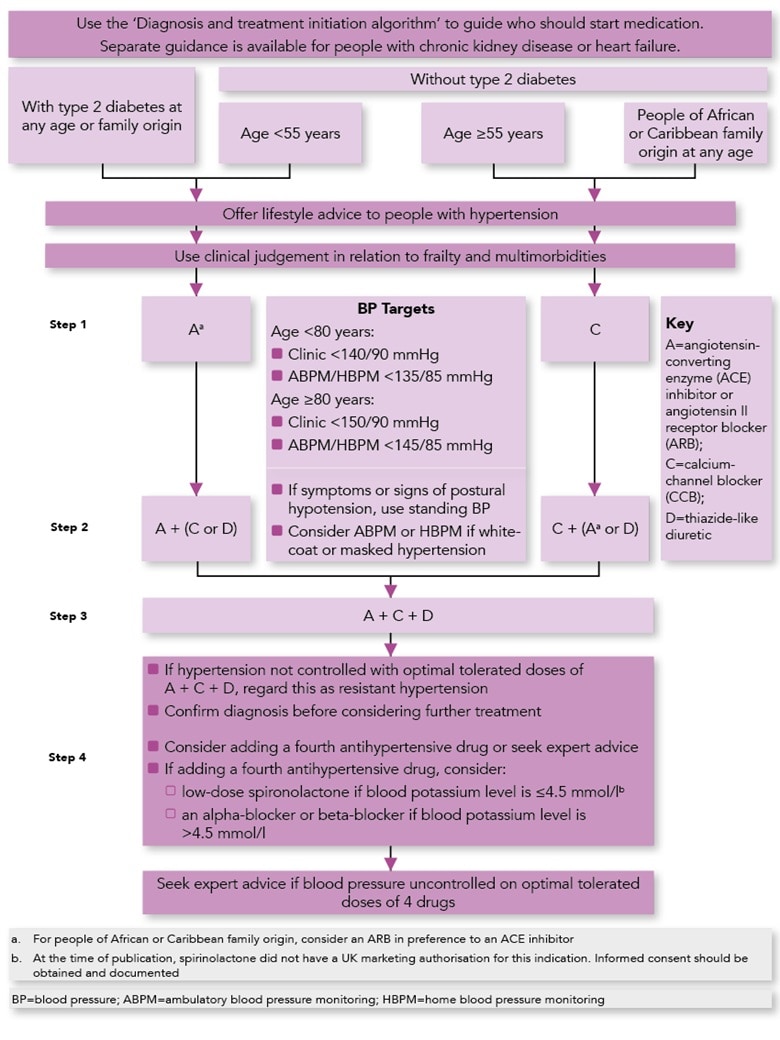
© NICE 2019. Hypertension in adults: diagnosis and management—draft for consultation, March 2019. Available from: www.nice.org.uk/guidance/indevelopment/gid-ng10054/documents All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication
After antihypertensive therapy has been initiated, the patient is invited back for an appointment with the practice pharmacist for a medication review and BP check. The review appointment usually takes place 4 weeks after treatment is started, but sometimes after 2 weeks if it is deemed urgent or there is clinical need. The pharmacist should assess response to treatment and review any adherence issues. If a patient is started on an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-II receptor blocker (ARB), they should also have their renal function and serum electrolytes checked before treatment initiation, and 1–2 weeks after treatment initiation or a dose increase.12
Medication Switches
The practice pharmacist can check for side-effects and adverse reactions and consider ways to address them. For example, a pharmacist prescriber could change the medication to another drug in the same class or switch the drug to a different class. The NICE algorithm for the treatment of hypertension (Figure 2) is a good resource to guide decision-making about which drug to prescribe.
Examples of medication changes include:
- switching a patient experiencing persistent dry coughs on an ACE inhibitor to an ARB
- stopping an ACE inhibitor or ARB if a patient has experienced angioedema, and switching to an appropriate alternative12
- if patients are experiencing ankle oedema on amlodipine, instead of adding a diuretic, they could be switched to lercanidipine as this is the dihydropyridine calcium-channel blocker that is the least likely to cause peripheral oedema.13
Drug Interactions
Practice pharmacists can also check if there are any drug interactions when reviewing medications. For example, certain antihypertensives (e.g. amlodipine, diltiazem) interact with simvastatin 40 mg, which can increase the risk of myopathy.14 The pharmacist can identify the risk, then facilitate a switch to a statin with a reduced risk of interaction with amlodipine (e.g. atorvastatin 20 mg) unless there are any contraindications.15
Annual Hypertension Review
Once BP has been optimised, the pharmacist can schedule the patient’s hypertension review for a year’s time, or earlier if clinically indicated. This will be picked up by the practice’s administration team to send out annual hypertension review invitations by post.
For patients with hypertension who have a stable BP within their target range, follow up should normally be done annually by a trained HCA or practice nurse. The 20-minute review consultation should include:
- measurement of:
- BP
- weight
- waist circumference
- assessment of general health
- reinforcement of non-pharmacological advice
- discussion about the patient’s lifestyle, symptoms, and (if applicable) medication, including adverse effects12
- renal function tests (serum creatinine, electrolytes, eGFR, and a urine dipstick to check for proteinuria):12
- if proteinuria is present, consider checking a patient’s urine albumin:creatinine ratio (ACR), which can also be managed by practice pharmacists.
A QRISK2 score should be calculated for patients not taking any statins for primary prevention of CVD. If the QRISK2 score is above 10%, they should have an appointment with the practice pharmacist to discuss starting statin therapy (usually atorvastatin 20 mg) for primary prevention of CVD.8,12
If a patient has resistant hypertension (i.e. they do not attain their BP target on optimal or maximum tolerated doses of four oral antihypertensives),3 then specialist advice should be sought. If a patient with hypertension becomes pregnant they should be offered referral to a specialist.16
The Role of the Practice Pharmacist
If a patient’s BP is confirmed to be persistently above the agreed treatment targets, the patient can be seen by the practice pharmacist to optimise BP control. Pharmacists can also take into account any abnormal blood test results, and refer to the GP where necessary. If patients have low BP readings and/or are experiencing hypotensive symptoms, they could also be referred to the practice pharmacist for a possible dose reduction, or complete stoppage, of oral antihypertensive medication with continual monitoring.12
Practice pharmacists may also titrate (up to the maximum tolerated doses) and monitor oral antihypertensive medications started in secondary care such as beta-blockers or ACE inhibitors for patients who may have had an acute coronary syndrome (ACS).17
Patients may become motivated to make lifestyle changes and they may want to reduce or stop using antihypertensive drugs. If the patient is at low cardiovascular risk and their BP has been well controlled for a number of years, they should be offered a trial reduction or withdrawal of therapy with appropriate guidance and be followed up for 6 months at 4-weekly intervals, then 2–3 times annually, to ensure any recurrence is detected.12 Patients vary in their attitudes to their hypertension and their experience of treatment. Details of patient organisations that provide useful forums to share views and information such as the British Heart Foundation or Blood Pressure Association may be helpful. It may be worth discussing exercise referral with the patient if clinically appropriate and the patient fits the relevant criteria.
Summary
Practice-based pharmacists can work successfully as part of the multidisciplinary general practice team to deliver excellent clinical care in the management of patients with hypertension. This has the potential to improve health outcomes for patients, provide value for money to practices (through meeting QOF indicators and cost-effective prescribing), while also significantly reducing the workload for GPs.
Pharmacists already have the necessary skills to manage patients with hypertension in patient-facing clinics, as clinical management is primarily based on managing medication and reducing inappropriate polypharmacy, as well as providing dietary and lifestyle advice to patients.18
Muhammad Siddiqur Rahman
Clinical practice-based pharmacist prescriber, trainee Advanced Clinical Practitioner, Court View Surgery, Kent; Board Member of the Pharmacist Cooperative

