Dr Richard Roope Provides Top Tips for GPs About Identifying Possible Colorectal Cancer and Supporting Patients to Reduce Risk and Achieve the Best Outcomes
| Read This Article to Learn More About: |
|---|
Find COVID-19 considerations and implementation actions for STPs and ICSs at the end of this article |
Colorectal cancer is the third most common cancer in both sexes in the UK (after breast and lung cancer in women, and prostate and lung cancer in men) with approximately 42,300 cases per year, and causing around 16,300 deaths per year.1 Over one-half of cases are preventable, and over one-half of patients diagnosed with colorectal cancer will live for 10 years or more beyond their diagnosis.1 Primary care has a role to play at almost every stage along the colorectal cancer pathway.
1. Offer Lifestyle Advice to Reduce Risk
In the UK, 54% of colorectal cancer cases are preventable each year,1 and primary care has a part to play in addressing some of the risk factors. In terms of numbers of cases that could be prevented by a change of lifestyle, colorectal cancer comes second only to lung cancer (see Figure 1).1 In all, 28% of cases of colorectal cancer are attributed to eating too little fibre, 13% are caused by eating processed meat, 11% are caused by being overweight or obese, 7% by smoking, and 6% by alcohol consumption.1 Offering very brief advice on lifestyle change is a simple, verified intervention that need not take more than 30 seconds.2
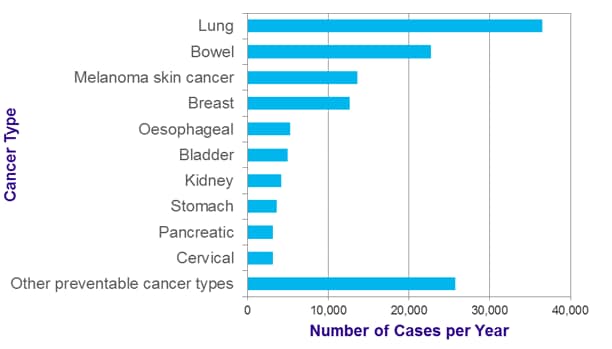
Credit: Cancer Research UK. Statistics on preventable cancers: preventable cancer cases by cancer type. www.cancerresearchuk.org/health-professional/cancer-statistics/risk/preventable-cancers#heading-One
2. Consider Aspirin to Reduce Risk in Lynch Syndrome
Lynch syndrome (LS), formerly known as hereditary non-polyposis colorectal cancer (HNPCC), is thought to affect around 175,000 people in the UK, but only 5% of cases are known.4 LS increases the risk of developing colorectal cancer by up to 80%, as well as increasing the risk of developing certain other cancers, such as womb and ovarian.4
NICE Guideline (NG) 151 on Colorectal cancer5 recommends: ‘Consider daily aspirin, to be taken for more than 2 years, to prevent colorectal cancer in people with Lynch syndrome.’ Evidence on the optimal dose is not yet clear; however, the guidance states: ‘commonly used aspirin doses in current practice are 150 mg or 300 mg.’5 It should be noted that use of aspirin for colorectal cancer risk reduction in people with LS is not currently licensed. The prescriber should follow relevant professional guidance, taking full responsibility for all clinical decisions. Informed consent should be obtained and documented. See the General Medical Council’s guidance on Good practice in prescribing and managing medicines and devices for further information.6
3. Encourage Patients to Take Up Screening
Colorectal cancer screening both prevents colorectal cancer by detecting adenomata and enables earlier diagnosis of colorectal cancer prior to the development of symptoms. Colorectal cancer screening was rolled out across the UK from 2007 (England) to 2010 (Northern Ireland), and saves 2400 lives per year.7,8 There is a significant deprivation gradient with take up (see Figure 2), although there is wide variation across CCGs of similar deprivation index. This is an example of the inverse care law; the demographic groups with the highest incidence of colorectal cancer are the groups who engage least with screening. GP endorsement of colorectal cancer screening has been shown to increase uptake.10 A new quality improvement (QI) domain on supporting early cancer diagnosis has been introduced for 2020/21, which gives general practices an opportunity to improve the uptake of bowel screening.11
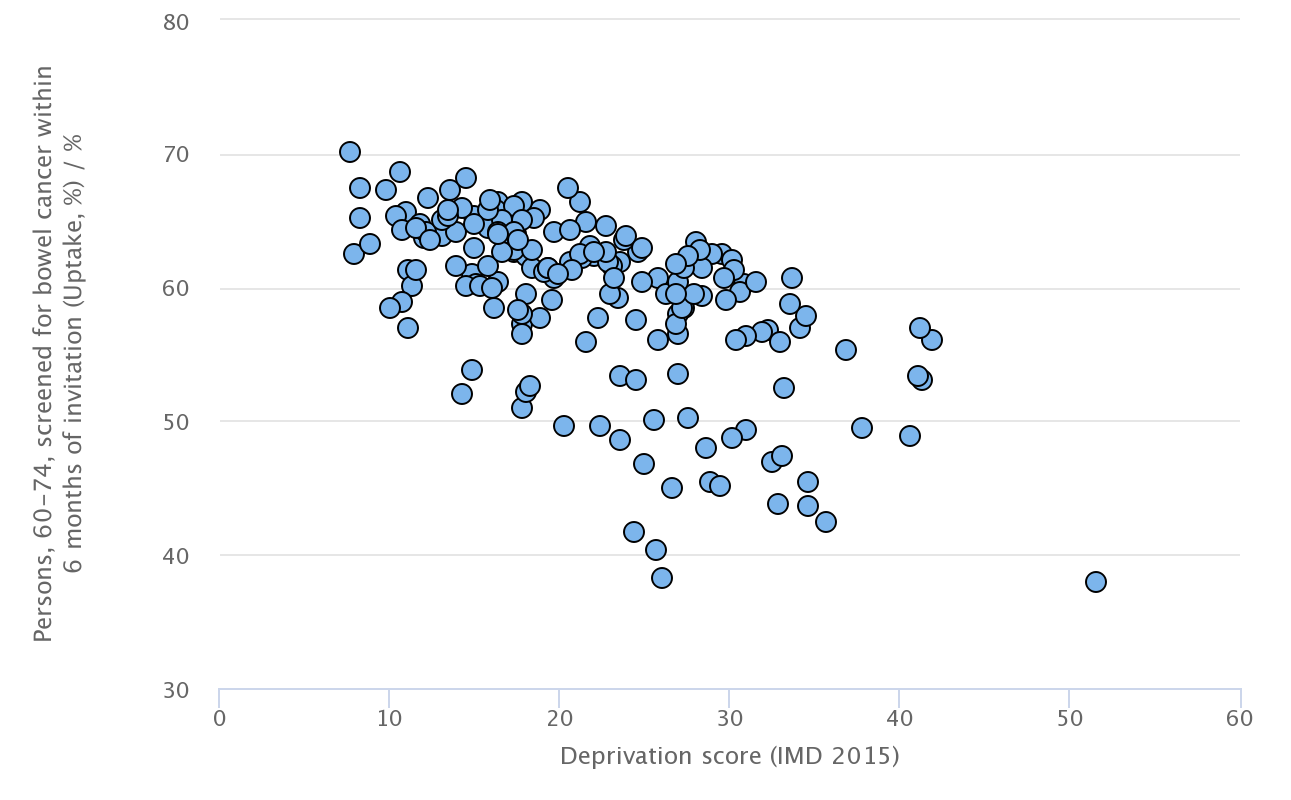
Public Health England. Cancer services. fingertips.phe.org.uk/profile/cancerservices/data#page/10/gid/1938132830/pat/46/par/E39000041/ati/165/are/E38000221/iid/91872/age/1/sex/4/cid/4/page-options/ovw-tdo-0_cin-ci-4Contains public sector information licensed under the Open Government Licence v3.0.
In 2011, the UK National Screening Committee recommended that a single bowel scope screening (flexible sigmoidoscope) be introduced for people aged 55 years. However, the roll-out of this has been slower than planned with only around 50% of those eligible invited, due to workforce constraints.8
4. Know the Local Eligibility Criteria for Screening
Screening ages vary across the four nations in the UK (see Table 1) so it is important to know the local eligibility criteria.12,13 Bowel scope screening, undertaken in a person’s 56th year, is being rolled out across England14 but the other three nations have not introduced this yet.
Table 1: Variations in bowel screening across the four nations in the UK
| Current Screening Age13 | Change to Screening from 50 Years | Option Over 74 Years13 | Telephone Number for Pack13 | Test12 | Change to FIT12 | FIT Screening Level12 | |
|---|---|---|---|---|---|---|---|
| England | 60–74 years | Commitment, but no date set15 | Yes | 0800 707 6060 | gFOBT | Underway from June 2019 | 120 mcg/g |
| Scotland | 50–74 years | Already implemented13 | Yes | 0800 012 1833 | FIT | Done | 80 mcg/g |
| Wales | 60–74 years | By April 202316 | No | N/A | FIT | Done | 150 mcg/g |
| Northern Ireland | 60–74 years | No commitment made | No | N/A | gFOBT | ‘Early 2020’ | N/A |
| gFOBT=guaiac faecal occult blood test; FIT=faecal immunochemical test | |||||||
5. Know the Different Thresholds for Screening Versus Symptoms
The faecal immunochemical test (FIT) is used at different thresholds for screening and symptomatic uses. The FIT is replacing the guaiac faecal occult blood test (gFOBT) for screening for colorectal cancer (see Table 1). In addition, the FIT is being introduced as part of the investigation of symptoms that can suggest colorectal cancer, as recommended in the NICE diagnostics guidance on Quantitative faecal immunochemical tests to guide referral for colorectal cancer in primary care.17 This is already embedded in most UK regions. Symptomatic FIT is recommended to guide referral for suspected colorectal cancer in people without rectal bleeding who have unexplained symptoms but do not meet the criteria for a suspected cancer pathway referral outlined in NG12 on suspected cancer.17,18 The testing threshold is set at 10 mcg/g—substantially lower than the screening threshold.17 It therefore remains important to investigate symptomatic patients who have had a recent ‘normal’ FIT screening result.
6. Have Easy Access to Guidance on Suspected Cancer
NICE Guideline 12 on Suspected cancer: recognition and referral18 was published in 2015 and slightly revised in 2017, and is the first NICE cancer guidance to be written by GPs for GPs. NG12 has had a part to play in the reduction of emergency presentations of cancer, which are recognised to have worse outcomes. Having ready access to NG12 allows for diagnosis of a higher proportion of cancers at an earlier stage of disease.
NG12 is different to other NICE guidelines in a number of ways: the recommendations are laid out by both anatomical zones and symptom presentations, and it standardises a universal minimum risk referral threshold of symptom and investigation findings of 3% across all cancers in adults. The result of this is that there are different age thresholds for different scenarios, which makes it almost impossible to remember them all. There are a number of helpful NG12 support resources produced by Cancer Research UK,19 Macmillan Cancer Support,20 and GatewayC (including a helpful interactive ‘mind map’ produced by Dr Ben Noble).21
The Scottish referral guidelines for suspected cancer22 were launched in 2019 and have many similarities to NG12.
7. Know the Age Thresholds for Different Symptoms
NICE Guideline 12 recommends specific age thresholds for different symptoms. GPs and other frontline clinicians should be aware of these to enable earlier diagnosis of colorectal cancer (see Box 1).18
© NICE 2017 Suspected cancer: recognition and referral. Available from www.nice.org.uk/guidance/ng12 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication
|
8. Remember that Patients are ‘Never Too Young’
Although 94% of cases of colorectal cancer occur in those aged 50 and over, across Europe the fastest rise in incidence of colorectal cancer is in 20–49-year-olds (see Figure 3).23,24
Clinicians should be aware that overall, European colorectal cancer incidence is rising in adults under the age of 50, who are not included in screening programmes. This phenomenon is the most significant in the UK, which has the highest annual percentage change of any of the countries studied.23 A good practice to adopt is one learnt in medical school: ‘three strikes and you’re in’; if a patient presents for a third time with the same colorectal symptoms, which have not responded to treatment, it may be appropriate to investigate further.
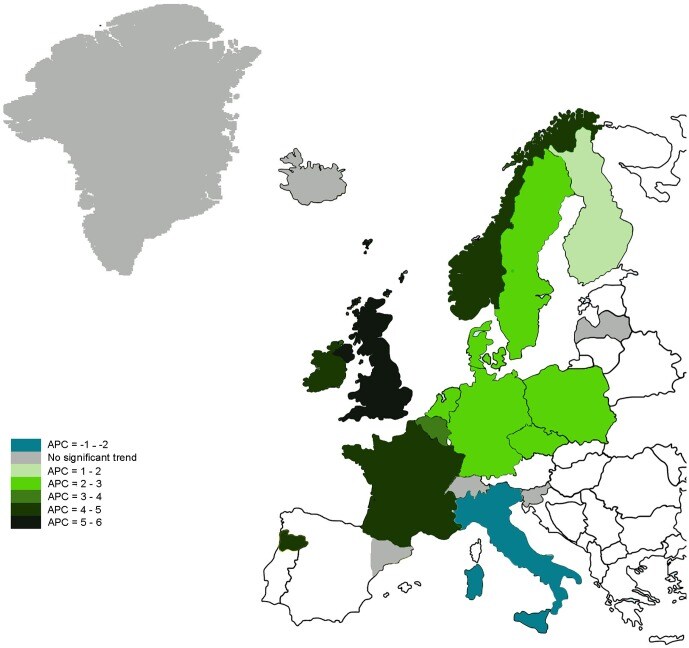
Vuik F, Nieuwenburg S, Bardou M et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 2019; 68 (10): 1820–1826.© Author(s) (or their employer(s)) 2019. Re-use permitted under CC BY 4.0. Originally published by BMJ.
9. Be Familiar with the Treatment Options
Patients diagnosed with colorectal cancer will be offered a growing number of treatment options. Primary care clinicians should be aware of these options, so they can support patients who may seek advice as part of their decision making. NG151 reviews the pros and cons of the various options for early stage colorectal cancer: transanal minimally invasive surgery, transanal endoscopic microsurgery, endoscopic submucosal dissection, and total mesorectal excision.5 For rectal cancers, most will be operated on laparoscopically except for locally advanced tumours, and those in people who have had multiple previous abdominal operations or previous pelvic surgery. Colon cancers will be treated either with laparoscopic or open excision, depending on the specifics of the tumour and the surgeon’s training and skill set. In people with metastatic colorectal cancer who are suitable for systemic anti-cancer treatment, genetic testing for RAS and BRAF V600E mutations will be undertaken.5
10. Be Aware of the Long-term Consequences
There are 268,000 people in the UK living with and beyond colorectal cancer.24 It is important to be aware of one of the long-term consequences of treatment: low anterior resection syndrome (LARS). LARS is a phenomenon seen in some people who have had sphincter preserving surgery. Symptoms include:5
- increased frequency of stool
- urgency with or without incontinence of stool
- feeling of incomplete emptying
- fragmentation of stool (passing small amounts little and often)
- difficulty in differentiating between gas and stool.
LARS is best assessed using the LARS score.5,25 The symptoms can be addressed with dietary management, laxatives, anti-bulking agents, anti-diarrhoeal agents, or anti-spasmodic agents.5 Where symptom control is not achieved to an acceptable level, secondary-care advice should be sought.5 This is best accessed, in the first instance, through the colorectal cancer Clinical Nurse Specialist.
Summary
Colorectal cancer is a major cause of morbidity and mortality in all developed countries, including the UK, and primary care clinicians have a big part to play in its prevention, early diagnosis, and survival. Outcomes have been improving over recent years; with some fairly simple interventions, improvements can be driven so much further, and towards matching the best outcomes in the world. This has become even more important in the COVID-19 pandemic, in which patients have been staying away from surgeries and screening has been put on hold. Primary care can make a difference to colorectal cancer outcomes, and the time for action is now.
Dr Richard Roope
Senior Clinical Advisor Cancer Research UK
GP, Whiteley, Hampshire
RCGP and Cancer Research UK Clinical Champion for Cancer 2014–2020
RCGP Clinical Advisor for Cancer
Member of the guideline development group for NG151
| COVID-19 Considerations |
|---|
|

