Dr Jez Thompson Navigates Liver Blood Test, including When to Request in Primary Care and How to Interpret the Results
| Read This Article to Learn More About: |
|---|
Find key points and implementation actions for STPs and ICSs at the end of this article |
For many major causes of death, including chest, neoplastic, and vascular disease, mortality is falling.1 However, deaths due to liver disease are rising rapidly; between 1970 and 2010 the UK standardised mortality rate for liver disease increased by over 400%.1 The mortality rate for patients under 65 years of age increased by almost 500% over the same period,1 and liver disease is now the fifth most prevalent cause of premature death in England and Wales.2
Liver disease in adults has three major causes: alcohol misuse; chronic viral hepatitis; and obesity/metabolic syndrome, which may lead to non-alcoholic fatty liver disease (NAFLD).3 Much liver disease is preventable and if it is diagnosed early, clinical interventions and lifestyle changes may slow or stop disease progression.3
In its early stages, liver disease is often asymptomatic—approximately 50% of patients with cirrhosis are first diagnosed when admitted to hospital with a decompensating event, such as ascites, bleeding varices, or hepatic encephalopathy.4
Primary care has a major role to play in the prevention and early detection of liver disease, and liver blood tests are an important aspect of this. In November 2017, the British Society of Gastroenterology (BSG) published Guidelines on the management of abnormal liver blood tests. The guideline is designed to be used in both primary and secondary care and includes recommendations on:3
- what constitutes an abnormal liver blood test
- how to respond to abnormal liver blood test results
- when liver blood tests should be performed
- what comprises a standard liver blood test panel.
Although traditionally referred to as liver function tests (LFTs), typical testing panels include measurement of hepatobiliary enzymes in addition to true measures of liver function. For this reason, the BSG guidance refers to liver blood tests rather than LFTs to capture more accurately the relevance to clinical practice.3
The Need for Guidance
There is no standardised panel for liver blood tests and testing varies between hospitals.3
Liver blood tests can be a challenge to interpret; results may be normal or near normal even in advanced liver disease, and, when abnormal, the degree of abnormality may not reflect disease severity—liver blood tests may be abnormal even when there is no significant liver disease.3 Standard liver blood test panels may be used routinely when patients have unexplained or non-specific symptoms and in these circumstances abnormal results are found in around 20% of patients.5 The significance of these results is often unclear and patients are frequently subject to further cycles of investigation, yet most patients referred to hospital with abnormal liver blood tests do not have significant liver disease.5
When to Perform Liver Blood Tests
Non-specific Symptoms
Liver disease can develop with few signs or symptoms, but using liver blood tests to investigate non-specific symptoms that may indicate liver disease, such as anorexia, fatigue, or nausea, may identify a hepatic condition that can be effectively treated.3 Using routine liver blood tests to investigate vague symptoms that do not point to possible liver disease may not be clinically helpful.
Evidence of Chronic Liver Disease
Liver blood tests, including international normalised ratio (INR), should be used to assess and monitor liver function in patients who have symptoms or signs of cirrhosis, portal hypertension, or liver failure. Signs and symptoms include ascites, peripheral oedema, spider naevi, and hepatosplenomegaly.3
Conditions Associated with a Risk of Developing Liver Disease
Patients with other autoimmune diseases are known to be at increased risk of developing autoimmune liver disease. Liver blood tests may, therefore, be appropriate if patients with autoimmune diseases develop symptoms that suggest liver disease, such as pruritus in primary biliary cholangitis.3
Additionally, patients with inflammatory bowel disease have just under a 10% risk of developing primary sclerosing cholangitis and should be considered for liver blood test monitoring.3
Use of Hepatotoxic Drugs
Because a wide variety of drugs have been associated with liver disease, liver blood tests may be recommended to monitor liver function in patients prescribed certain medications such as carbamazepine, methyldopa, minocycline, macrolide antibiotics, nitrofurantoin, statins, sulphonamides, terbinafine, chlorpromazine, and methotrexate.3
Although statins can lead to drug-induced liver injury this is rare, and studies have demonstrated that statins are generally suitable for use in patients with pre-existing abnormal liver enzymes.3
Family History of Liver Diseases
Patients who have relatives with familial diseases, including haemochromatosis or Wilson’s disease, should be screened for these conditions with relevant tests.3
Alcohol Misuse
Liver enzymes are of little value in assessing the extent of alcohol misuse, and are a poor guide to the development of progressive fibrosis in alcohol-related liver disease (ARLD). Elevated enzymes may, however, be useful in motivating behaviour change, with elevated gamma-glutamyltransferase (GGT) being the best predictor of mortality.3 NICE Guideline (NG) 50 on Cirrhosis in over 16s: assessment and management recommends screening for cirrhosis using transient elastography in patients who have been drinking at harmful levels (in excess of 50 units per week and 35 units per week for men and women, respectively) for several months.6
Viral Hepatitis
Chronic viral hepatitis may be associated with non-specific symptoms, including fatigue, but most patients are symptom-free. Tests for hepatitis B and/or hepatitis C are recommended when risk factors are identified and as part of a liver aetiology screen when liver blood tests are abnormal. Risk factors for hepatitis include:3
- birth or upbringing in a high-prevalence country
- a history of injecting drugs
- close household contact with someone with viral hepatitis
- time spent in prison.
Risk Factors for Non-alcoholic Fatty Liver Disease
Normally suspected following abnormal liver blood tests or an echobright liver on ultrasound scan, non-alcoholic fatty liver disease (NAFLD) is, in part, a diagnosis of exclusion. When fatty change is seen on ultrasound, other causes including alcohol misuse and viral hepatitis, should be considered.3 NICE Guideline 49 on Non-alcoholic fatty liver disease (NAFLD): assessment and management recommends that liver bloods tests should not be used to rule out NAFLD in those with risk factors such as obesity and metabolic syndrome.7
Interpreting Test Results
The BSG guidelines3 include information on a range of different liver blood tests, providing guidance on how test results should be interpreted and making recommendations for further investigations that may be appropriate.
Bilirubin
Most laboratories report total bilirubin, which will be raised by an elevation of either the conjugated or the unconjugated form. In adults, the most likely cause of an isolated raised unconjugated bilirubin, once haemolysis has been excluded, is Gilbert’s syndrome—an inherited metabolic disorder characterised by impaired conjugation, which is not associated with liver disease.3 Raised conjugated bilirubin is seen in obstruction of the hepatobiliary system or in parenchymal liver disease, such as hepatitis from any cause or advanced cirrhosis.3
Interpretation of hyperbilirubinaemia in neonates and infants requires specialist support because of the risk of kernicterus and the need to diagnose with urgency conditions such as biliary atresia.8
Albumin
Albumin is a protein synthesised by the liver that can serve as a marker of synthetic liver function. Albumin concentration may, however, be reduced in other clinical situations, including sepsis, systemic inflammatory disorders, nephrotic syndrome, malabsorption, and gastrointestinal protein loss.3
Alkaline Phosphatase
Alkaline phosphatase (ALP) is predominantly a liver enzyme but is also found in bone and in smaller quantities in the intestines, kidneys, and white blood cells. Levels of ALP are higher in childhood and in pregnancy, where it is associated with bone growth and placental production, respectively.3 Consequently, pathologically increased levels of ALP may be found not only in cholestatic liver disease (e.g. common bile duct obstruction, intrahepatic duct obstruction [including by metastases], primary biliary cholangitis, primary sclerosing cholangitis, and drug-induced cholestasis) but also in bone disease (metastatic bone disease, vitamin D deficiency, Paget’s disease, and bone fractures). Raised ALP may also result from cholestasis caused by hepatic congestion due to right-sided heart failure.3
If ALP is elevated in isolation, measurement of GGT (see below) can help to provide some indication as to whether or not the origin is hepatic, and, if doubt remains, electrophoresis can be used to differentiate hepatic from non-hepatic ALP.3
Aspartate Aminotransferase and Alanine Aminotransferase
Elevated levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are the most common abnormalities seen in liver blood tests. Both AST and ALT are enzymes present in hepatocytes that are released into the blood following hepatocyte injury or death.3 Alanine aminotransferase is present at low concentrations in non-hepatic tissue and elevations that are not liver-related are uncommon. In contrast, AST is present in cardiac, smooth, and skeletal muscle and may be elevated in myocardial infarction or myositis. Although AST is not as liver-specific as ALT, it may be a more sensitive indicator of liver cell injury.3
In children, creatine kinase measurement may help to determine whether an isolated rise in either of these two enzymes is due to an underlying skeletal muscle disorder, such as muscular dystrophy.3
Gamma-glutamyltransferase
Abundant in the liver and also present in the intestines, kidneys, pancreas, and prostate, but not in bone, GGT can be useful in determining whether elevated ALP is of bone or liver origin. Levels of GGT may be elevated by factors that are not liver-related, including obesity, excess alcohol consumption, and certain drugs. In spite of this low specificity, GGT is one of the best predictors of mortality in liver disease.3
As ALP is not a reliable indicator in children, GGT can be used to establish the likelihood of biliary disease, for example congenital abnormalities of the biliary tract and genetic disorders of bile metabolism.3
Coagulation Tests
Prothrombin time (PT) and international normalised ratio (INR) are measures of blood clotting. Clotting factors are synthesised in the liver and, when there is significant liver damage (usually >70% loss of synthetic function), their production is reduced, which may be demonstrated by prolonged PT or INR. Prolonged PT or INR can, therefore, indicate acute or chronic liver dysfunction, but can also be caused by vitamin K deficiency in fat malabsorption and chronic cholestasis.3
Platelets
Platelet reduction is an indicator of advanced liver disease, although platelets may be reduced in a wide variety of medical conditions. In liver morbidity, platelet reduction is associated with splenic enlargement secondary to portal hypertension with consequent platelet sequestration; a reduction in thrombopoietin levels; and reduced platelet production.3
Abnormal Test Results
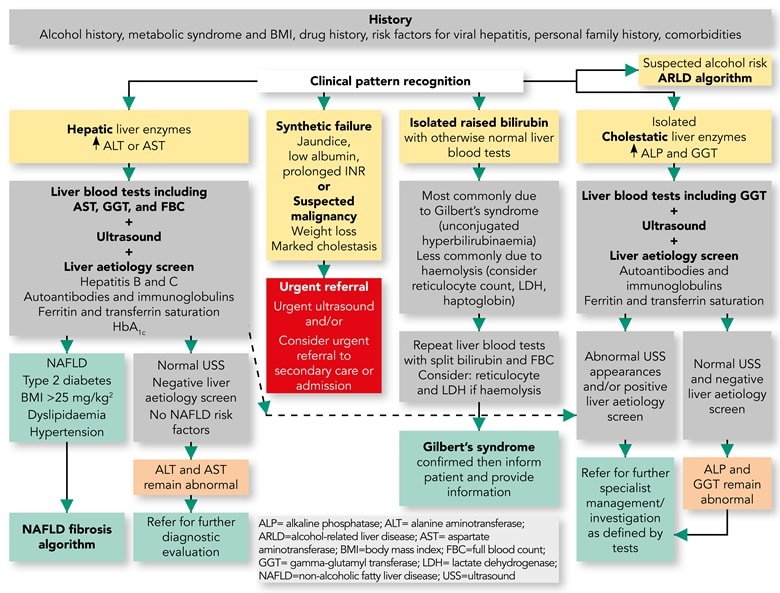
When results of liver blood tests are abnormal, the clinical response should include: obtaining a thorough clinical history; performing examinations; and, in appropriate patient groups, considering primary sclerosing cholangitis and viral hepatitis (see Box 1 and Figure 1).3
| Box 1: Clinical Responses to Abnormal Liver Blood Tests3 |
|---|
ALT=alanine aminotranferase |
Source: Newsome P, Cramb R, Davison S et al. Guidelines on the management of abnormal liver blood tests. Gut 2018; 67 (1): 6–19.
Reproduced under the terms of the CC BY 4.0 license.
This figure details the initial response to abnormal liver blood tests. Boxes in yellow indicate the initial evaluation of the clinical presentation. Patients with marked derangement of liver blood tests, synthetic failure and/or suspicious clinical symptoms/signs should be considered for urgent referral to secondary care (red box). For the remainder, a clinical history alongside evaluation ofthe pattern of liver blood test derangement will determine choice of pathway and is shown in the grey boxes. A grey box indicates all the tests that should be requested at that stage rather than a hierarchy within it. The presence of metabolic syndrome criteria should be sought to support a diagnosis of NAFLD. For children, the [guideline] text should be consulted for modification of recommendation. Areas of diagnostic uncertainty are indicated in orange boxes and the decision for repeat testing or referral to secondary care will be influenced by the magnitude of enzyme elevation and clinical context. Green boxes indicate final/definitive outcomes for users of the pathway.
*Abnormal USS may well include extrahepatic biliary obstruction due to malignancy, which should result in urgent referral. ALP=alkaline phosphatase; ALT=alanine aminotransferase; ARLD=alcohol-related liver disease; AST=aspartate aminotransferase; BMI=body mass index; FBC=full blood count; GGT=gamma-glutamyltransferase; INR=international normalised ratio; LDH=lactate dehydrogenase; NAFLD=non-alcoholic fatty liver disease; T2DM=type 2 diabetes mellitus; USS=ultrasound scan
Approaches to Common Conditions
Non-alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease is most commonly suggested by an echobright liver on ultrasound and other causes of fatty changes in the liver, including alcohol misuse, must be excluded in order to establish the diagnosis.3
Once NAFLD has been diagnosed, the BSG guideline recommends screening for advanced fibrosis using a non-invasive, algorithm-based assessment that brings together serum and other biomarkers. Examples include Fibrosis-4 (FIB-4) or NAFLD fibrosis score (NFS).3 NICE Guideline 49 recommends considering the enhanced liver fibrosis (ELF) test for this purpose.7
Patients with NAFLD who do not have advanced fibrosis can be managed in primary care, with treatment focusing on:3
- long-term weight loss through reduced calorie intake and increased physical activity
- management of co-morbidities, including diabetes, dyslipidaemia, and hypertension.
Where tests indicate advanced fibrosis the patient should be referred to a hepatologist.3
Alcohol-related Liver Disease
Alcohol-related liver disease is the most common cause of liver-related mortality in western populations. Most patients with ARLD drink heavily, but ARLD is not limited to those who are dependent on alcohol. A relationship also exists with obesity—the risk of liver disease doubles for any given alcohol intake when body mass index exceeds 35 kg/m2.3
Prevention and treatment of ARLD is focused on helping patients to stop drinking harmfully.3 Brief alcohol interventions in primary care are effective at lower levels of alcohol misuse, but those who are unable to address their drinking or who are dependent on alcohol should be referred to alcohol services.
Conclusion
Primary care clinicians have an important role in the prevention, early diagnosis, initial investigation, and referral of patients with liver disease. There are, however, challenges associated with this, including:
- the large number of patients with risk factors for developing liver disease
- limited time available for GPs and practice nurses
- lack of confidence in delivering brief interventions for alcohol and obesity
- availability of referral pathways for patients who misuse alcohol or who are obese
- investigations, including ELF and transient elastography testing, being difficult to access.
Appropriate use of liver blood tests can support early diagnosis and the identification of risk factors for liver disease. This in turn enables the use of early interventions to stop liver disease developing, or prevent early liver disease progressing to cirrhosis. The BSG guidance on liver blood tests provides recommendations on choosing appropriate liver blood tests, interpreting the results, and subsequent actions, which it is hoped will support the important role of primary care in preventing and identifying liver disease. For sources of further information, see Box 2.
| Box 2: Information for Patients, Carers, and Practitioners |
|---|
The website of the British Liver Trust (www.britishlivertrust.org.uk) provides comprehensive information both for healthcare professionals and for patients with liver disease. |
Dr Jez Thompson
RCGP/British Liver Trust Clinical Champion for Liver Disease Clinical Director, Bevan Healthcare
| Key Points |
|---|
NAFLD=non-alcoholic fatty liver disease |
| Commissioning Messages |
|---|
Written by Dr David Jenner, GP, Cullompton, Devon
BSG=British Society of Gastroenterology; NAFLD=non-alcoholic fatty liver disease; FIB-4=fibrosis-4; NFS=NAFLD fibrosis score |

